The US healthcare administration is one of the best developers of comprehensive patient databases. And those databases are a goldmine for healthcare research; they permit large-scale retrospective longitudinal cohort studies to be performed, and can help reveal nuggets like never-before-noticed associations between one disease and another.
To this end, Woodward et al. (1) mined the Clinformatics DataMart database (OptimumInsight), which contains detailed records on all insured patients (nearly 16 million) in a large, nationwide, US managed care network over a 12-year period spanning from January 1st 2001 to December 31, 2012. The purpose? They wanted to establish if a link exists between common systemic diseases, sociodemographic factors, and keratoconus. In there, they identified 16,053 patients who had been diagnosed with keratoconus on two or more separate occasions, and a further 16,053 matched controls, from which they could begin to identify sociodemographic factors and common systemic diseases that were associated with the development of keratoconus. The sheer size of their dataset was a considerable advantage over many previous studies on the same topic, which had sample sizes ranging from just 25 to 1,529 patients.
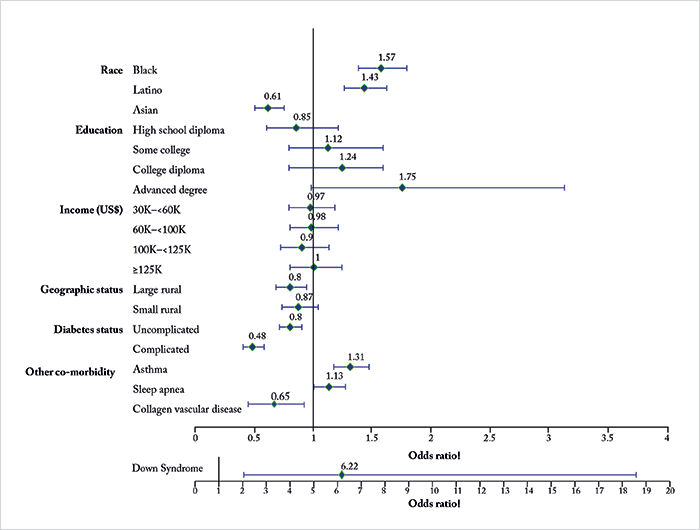
What they found confirmed some previously-found associations, but contradicted others (Figure 1). For example, the odds of a person being diagnosed with keratoconus varied by race – relative to White people, Black and Latino people had higher odds of developing keratoconus (by 57 percent and 43 percent, respectively), whereas Asian American people were less likely to develop the disease (by 49 percent). Considering the impact of systemic disease, those with diabetes mellitus and collagen vascular disease were less likely to have keratoconus (see Figure 1), whereas people with asthma, sleep apnea, and Down syndrome were considerably more likely to receive a diagnosis. Education status and income level had no significant effect, however people living in large, rural communities had a 20 percent lower odds of having the disease. So what do the study’s authors think is going on? The observation of a decreased risk of keratoconus in American patients of Asian ethnicity contradicts previous findings (from smaller studies) that suggest that Asian people are at a greater risk of developing the disease. The fact that patients from rural areas were 20 percent less likely to be diagnosed with keratoconus might arise from the fact that fewer corneal specialists are present in rural areas, and this might mean that patients with mild or form fruste disease go undetected. With diabetes, it’s possible that elevated levels of (the highly reactive ketone) glucose can lead to glycosylation and cross-linking of the cornea, thereby strengthening it – and if a patient has diabetes complicated by end-organ damage, this is suggestive of even poorer glucose control (and even greater circulating levels). While the authors do not propose potential causative reasons for the association between asthma and sleep apnea with a keratoconus diagnosis, they do note that it’s probably appropriate to ask patients with keratoconus if they are experiencing breathing difficulties, as this might reveal cases of undiagnosed asthma. Similarly, screening for sleep apnea, initially with the Berlin questionnaire, should be considered.
References
- MA Woodward et al., “The association between sociodemographic factors, common systemic diseases, and keratoconus: an analysis of a nationwide heath care claims database”, Ophthalmology, 123, 457- 465.e2 (2016). PMID: 26707415.
