- Phacoemulsification in patients with corneal opacity can be a challenge – patients with central but superficial opacity and concomitant cataract are common, yet do not typically require a full-thickness transplant
- Conventional lamellar keratoplasty has issues, too – problems such as infection and suture-related astigmatism can make outcomes unpredictable
- The use of biological glue to adhere the graft to the host cornea can bypass the problem of sutures, and has seen success when performed as a standalone procedure for treating corneal opacity
- Combining cataract surgery with automated sutureless anterior lamellar keratoplasty can provide rapid vision rehabilitation, and make phacoemulsification more straightforward for the surgeon
Performing phacoemulsification in a patient with corneal opacity is a challenge, even for an experienced cataract surgeon. Often, we come across patients with central but superficial opacities, and concomitant cataract, who do not warrant a full thickness keratoplasty. One option for these patients is a combined surgery, with a lamellar graft and phacoemulsification. However, conventional lamellar keratoplasty has its own problems, such as suture-related astigmatism and infections, and can be unpredictable.
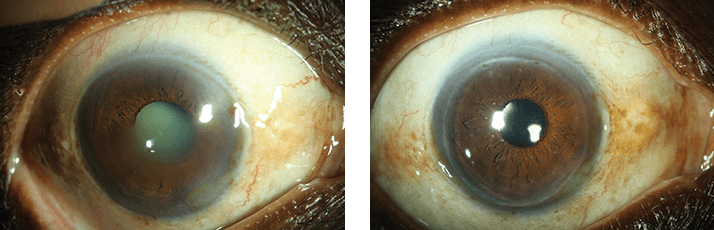
But there is a way to bypass the problem of sutures – using a biological glue to stick the graft to the host cornea. The results we have witnessed so far of sutureless lamellar keratoplasty, performed as a standalone procedure for the management of corneal opacities, have been encouraging (see Figure 1).
The why and the how
We decided to combine cataract surgery with microkeratome-assisted sutureless anterior lamellar keratoplasty in eyes with visually significant corneal opacity involving less than 200 µm of anterior stroma. This approach enables rapid visual rehabilitation after a single combined surgery (rather than a staged procedure). The residual stromal bed is thick and smooth – which means performing phacoemulsification is less surgically challenging. In terms of technique, sutureless corneal transplantation can best be described as replacing the ‘free LASIK cap’, with the cap being taken from a donor cornea. We performed this triple procedure (lamellar keratoplasty, phacoemulsification and IOL implant) in seven eyes of six patients with anterior stromal corneal opacity. All the procedures were carried out under peribulbar anesthesia, and a Moria microkeratome and artificial chamber (ALK System, Moria) with a 200 µm microkeratome head. For trephination of the host cornea, a suction ring (number 0) was placed over the host cornea, and the same microkeratome head (200 µm) was used to trephine the recipient bed. Phacoemulsification was completed through a 2.7 mm superior incision, and the donor lenticule was then placed on the host bed and any residual fluid from the groove at the graft-host junction was absorbed using merocel sponges. One drop of slow component (thrombin 4) fibrin sealant (Tisseel, Baxter Healthcare) was evenly spread along the edges of the donor cornea, into the groove. No adhesive was applied over the stromal bed. The glue was allowed to act for a period of three minutes, and following this, any excess coagulated glue was removed using the sponge wick. A bandage contact lens was then placed over the cornea and retained for a period of three weeks.Better together?
The results were promising. Mean topographic and refractive astigmatism were 2.77 ± 2.6 D and 1 ± 0.65 D, respectively at six months of follow-up. The mean spherical equivalent was -0.7 ± 1.31 D, with a range of -2 D to +1.38 D. Owing to irregular corneal surface and haze, the pre-operative keratometry and refraction could not be assessed. The mean gain in uncorrected visual acuity was 7.1 ± 4 lines, and 8.8 ± 3.4 lines in best corrected visual acuity (BCVA), with four eyes having best spectacle-corrected visual acuity (BSCVA) ≥ 20/40. There were no cases of graft dislocation, infection, vascularization or recurrence of primary pathology. One eye developed epithelial ingrowth (small and peripheral), and the same eye also developed acute graft rejection – but this problem was reversed completely using topical steroids. Overall, we believe this method offers many advantages. The removal of the superficial flap at the beginning of surgery clears up the host cornea, and, as a result of the enhanced visibility of intraocular structures, this step makes the subsequent phacoemulsification significantly easier. Following the cataract surgery, graft application using glue takes only a few minutes. Our surgical technique also allows early tapering of topical medications, which may improve patient compliance and quality of life in comparison to keratoplasty using sutures. As patient demands for early visual rehabilitation continue to increase, we believe combining these two proven but independent surgical techniques addresses an unmet need.Tips and tricks
There are certain tips that we would like to offer to those considering adopting this approach. First, we recommend that the same surgeon should cut both the host and donor cornea, the reason being there is an inter-person variability while cutting the cornea, so if two different surgeons work on the host and donor, disparity between them is likely. Second, when the graft is being attached, the interface between the host and donor cornea must be dried thoroughly, similar to the way this is done in a LASIK case (i.e. using two merocel sponges). Finally, remember to apply a bandage contact lens in each case. We have found this surgery to be easily repeatable, with consistent results, and we believe that the fast visual rehabilitation it offers will result in its widespread adoption in the future.Tushar Agarwal is additional professor of Ophthalmology, All India Institute of Medical Sciences, New Delhi, India. He has over 60 published papers, including more than 15 new surgical techniques. Pooja Bandivadekar is a Consultant Cornea, Cataract and Refractive Surgeon at the Doctor Eye Institute, Mumbai, India.
