- Ocular glaucoma drops, while effective, are plagued by lack of compliance
- Patients and clinicians are looking for an alternative to traditional, high-risk surgical options
- CO2 lasers are highly effective for ablation of dry tissue and are absorbed by liquid
- This makes CO2 laser-assisted sclerectomy surgery (CLASS) a safe and precise treatment option
Glaucoma is the second most common cause of blindness globally. Currently, an estimated 8.4 million in the world are blinded by the disease, with a further 60 million affected by optic neuropathy (1), and these numbers will only increase. There is therefore an urgent need for improved understanding of the underlying pathology and better treatment options that this knowledge will give rise to. Thankfully, headway is being made.
Traditional treatment for glaucoma begins with topical hypotensive medications. These prevent nerve damage when used according to their prescription (2) but are much less effective for the high percentage of patients that are not fully compliant. Studies have shown that only around 46 percent of patients fulfill all of their prescriptions (3), and of those that do, less than 30 percent are instilling them correctly (4). For a disease in which the only course of treatment is to prevent ocular nerve damage, this is not good news. The traditional surgical alternatives, such as trabeculectomy and tube shunts, come into play only when the disease state is dire enough to exceed the high risks associated with surgery.
A new surgical option
In the last few years there has been a surge of surgical alternatives as clinicians and scientists search for low- risk, high-efficacy treatment options. The approach that I have helped to develop within this niche is CO2 laser-assisted sclerectomy surgery (CLASS). Although CO2 lasers are well-known in the field of general surgery, especially plastic surgery, it took a laser manufacturing company, Optomedic, to bring the benefits of the CO2 laser to my attention back in 1998. This laser is unique in that it is highly effective for dry tissue ablation while being almost completely absorbed by liquid; it is therefore not suitable for any intraocular procedure. We hypothesized that it would be possible to ablate the dry sclera over the Schlemm’s Canal and trabecular meshwork until the tissue became thin enough to allow fluid to percolate out through the tissue. The percolating fluid would absorb any additional laser energy, preventing further ablation of the tissue that may lead to penetration into the eyeball. When we studied the tissue effect of the CO2 laser on a variety of animal and human cadaveric eyes and on living rabbits, the hypothesis was supported in these near-clinical settings: fluid percolation was achieved in all cases whereas penetration into the anterior chamber occurred in only about five percent of cases.Our CLASS procedure was subsequently developed using IOPtiMate (IOPtima, Israel), a unique system that consists of a CO2 laser with a wavelength of 10.6 µm (infrared), accompanied by a micro-manipulating scanner that uses an aligned HeNe laser aiming beam (red; 632 nm), and a control unit. The CLASS procedure is as follows (see Figure 1):
- A peritomy and superficial scleral flap dissection is made, which extends to the clear cornea.
- At the discretion of the physician, 0.02–0.04% Mitomycin C can be applied for 1–3 minutes after the creation of the scleral flap.
- The red aiming beam is used to identify and confine the laser ablation zone distal to the limbus.
- The laser ablation is aimed at the zone directly above Schlemm’s canal and scleral tissue is removed layer by layer until fluid percolates through the tissue.
- The Laser ablation effect “automatically” stops as aqueous begins to percolate, that is, when the desired end-point is achieved.
- Once sufficient sclera has been ablated and the aqueous percolates effectively, the scleral flap is replaced and sutured.
CLASS reduces elevated intraocular pressure (IOP) in patients with primary open angle glaucoma (POAG) and pseudo exfoliative glaucoma (PEXG) by thinning, but leaving intact, the sclera of the eye, thus improving drainage without penetrating the eye globe. Aqueous flow is successfully regenerated using nature’s own pathways and with no need to insert any foreign drainage devices.
Results to date
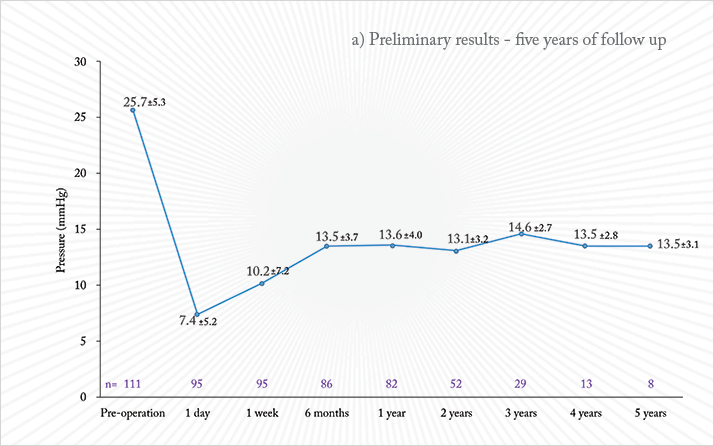
In initial clinical studies performed in 2003–2004 with the CLASS procedure immediate success was seen in all cases; however, about one-half of the cases failed during follow-up, because of tissue scarring. The initial laser parameters had been set at low energy and long exposure time, essentially performing less tissue ablation and more photocoagulation. Appropriate adjustments were made to the laser parameters. We now have data for up to five years on human eyes using the third generation of the IOPtimate system. In a prospective, multi-center study of 111 patients, the procedure was performed on 85 eyes with POAG and 26 eyes with PEXG and an average IOP of 25.7 +/- 5.3 mmHg. Mean IOP (see Figure 2a) dropped to 13.5 +/- 3.7 mmHg at six months post-operative (N=86) and remained stable through three years (N=29) and five years post-operative (N=8). The average number of hypotensive medications (Figure 2b) dropped from a mean of 2.3 +/- 1.2 at baseline to 0.3 +/- 0.7 at six months post-operative, 0.6 +/- 0.8 after three year and 0.8 + 1.0 after five years. At three years post-operative, 87.5 percent of patients achieved a reduction in IOP of 20 percent or greater, maintaining an IOP less than or equal to 18 mmHg; 59.4 percent of patients were able to maintain the IOP goals without use of any medication. Mitomycin C was used in 93 percent of procedures.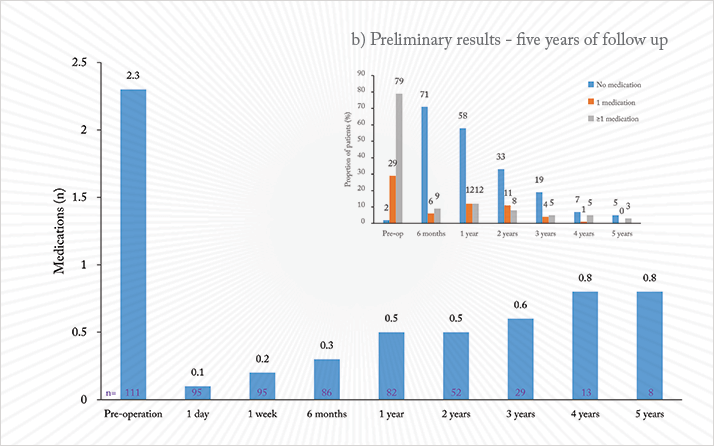
CLASS is appropriate for patients with mild to moderate POAG and PEXG, aiming to serve those patients with baseline IOP between 20 mmHg and 35 mmHg and possibly even higher. It is also suitable for combination with cataract surgery. Patients with mild to moderate glaucoma are often seen by comprehensive-care ophthalmologists rather than by glaucoma specialists, and the precision of the CLASS procedure makes it a solution that is very accessible to all surgeons. The laser beam is precisely guided by the micro-manipulating beam, and will ablate exactly what is chosen according to the defined shape and dimensions; physicians simply have to exercise confidence in the device. Keeping the eye intact significantly reduces the risk of intra-operative and post-operative complications and the follow-up interventions commonly associated with penetrating surgical alternatives.
In multi-center clinical studies and in commercial practice, the approach is highly effective at lowering IOP, and in reducing hypotensive medication as well as resulting in lower post operative complications. CLASS has received regulatory approvals in Europe (CE), Mexico, Israel and is soon to be approved in China. So far, approximately 700 procedures have been performed worldwide. Ehud Assia is the Director of the Department of Ophthalmology, Sapir Medical Center, Meir Hospital, Kfar Sava, Israel.
References
- C. Cook, P. Foster, “Epidemiology of Glaucoma: What’s New?” Can. J. Ophthalmol., 47,223–226 (2012). M.A. Kass et al., “The Ocular Hypertension Treatment Study: A Randomized Trial Determines That Topical Ocular Hypotensive Medication Delays or Prevents the Onset of Primary Open-Angle Glaucoma,” Arch. Ophthalmol., 120, 701–713 (2013). D.S. Friedman et al., “Using Pharmacy Claims Data to Study Adherence to Glaucoma Medications: Methodology and Findings of the Glaucoma Adherence and Persistency Study (GAPS),” Invest. Ophthalmol. Vis. Sci., 48, 5052–5057 (2007). J.L. Stone et al., “An Objective Evaluation of Eyedrop Instillation in Patients with Glaucoma,” Arch. Ophthalmol., 127, 732–736 (2009).
