The sudden cancellation of millions of elective surgeries globally as a result of the COVID-19 pandemic (1) has created a substantial backlog of cataract procedures for ophthalmologists – and plenty of hurdles to overcome before we can get anywhere close to “practice as usual.”
As surgical centers begin to clear this unenviable backlog, it is more important than ever to understand and minimize all possible routes of infection during surgery. Although various infection control and personal protective equipment (PPE) measures recently recommended for ophthalmologists have shown decreased transmission rates during clinic visits (2, 3), they have not specifically taken the OR into account. Nonetheless, we must make sure we’re protected.
We are exposed
Increased COVID-19 transmission is related to extended exposure time; although the exact infectious dose remains unclear, it has been estimated that infection could be possible after roughly five minutes speaking with an infected person (4). Ophthalmologists spend prolonged periods of time in close proximity to a patient’s mucosal membranes when performing surgery, so it stands to reason that this could increase the risk of contracting COVID-19.
Movement in, out, and around the OR can also be problematic. Have you ever felt the need to apply caution when unfolding PPE, such as a surgical gown or drape? Research reveals that, even when appropriate PPE is used to standard protocols, the unfolding process could generate a large number of potentially infectious airborne particles (5). OR staff turnover is also considered risky; surgical site infection rates have been shown to decrease in hospitals with lower turnover (5). Ophthalmology is a surgical specialty with a very high case turnover rate, resulting in increased foot traffic and drape or gown movement throughout the day – and an even greater risk of viral transmission.
Finally, it’s possible that ophthalmologists will work even longer hours in a bid to clear the strenuous, pandemic-induced backlogs of cataract surgeries. Health authorities may even increase the volume of surgeries conducted, for instance by allowing OR time during weekends. So, it’s essential for us to examine all possible infection risks in the OR and make every effort to mitigate them.
Condensation capped
At the time of writing, TLC Laser Eye Centers in Oakville, Ontario, had performed over 80 routine phacoemulsification and intraocular lens (IOL) implantation surgeries since a return from the COVID-19 hiatus.
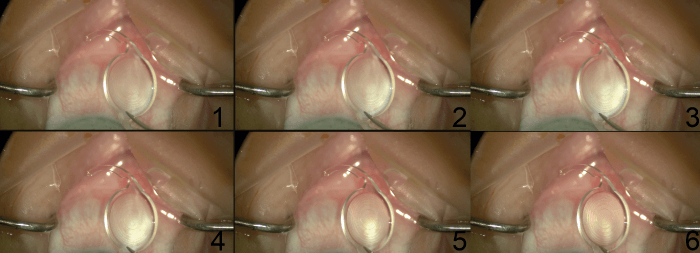
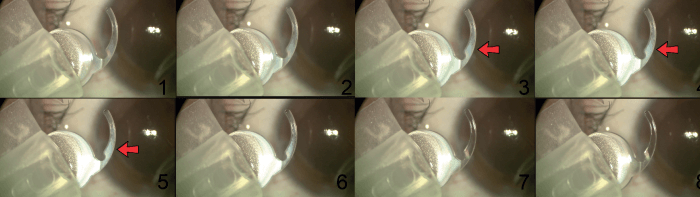
During surgery, we observed condensation appearing on the IOL when it was placed 1 cm above the patient’s eye just prior to insertion, in sync with the patient’s breathing (Figure 1). After seeing the same scenario play out in many cases, we realized that the condensation was an indicator of air leakage from underneath the surgical drape seal around the patient’s eye, so we began to test the integrity of the seal.
Why was it important to do that? Leakage of a patient’s breath could increase the infection risk of COVID-19 from patient to ophthalmologist, especially if that patient were to sneeze or cough, as demonstrated in a simulated ophthalmology OR setting (6).
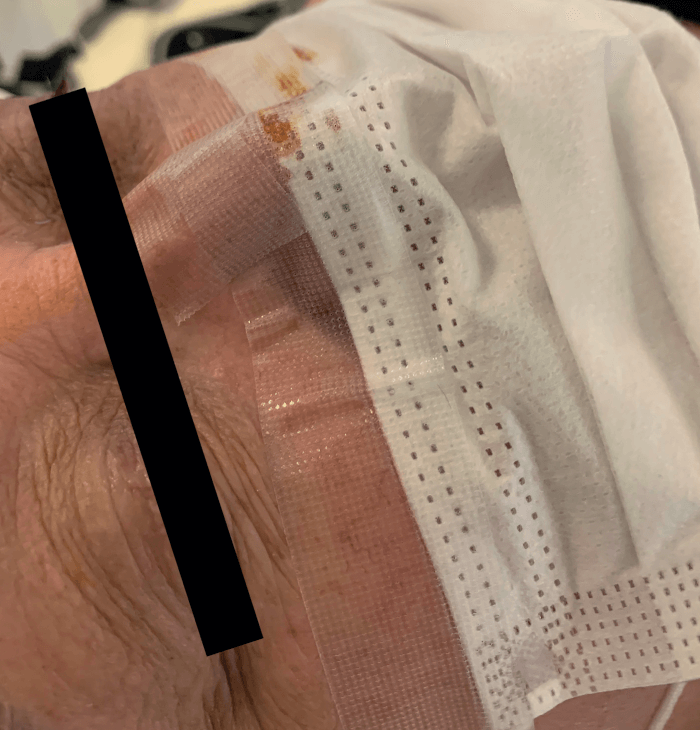
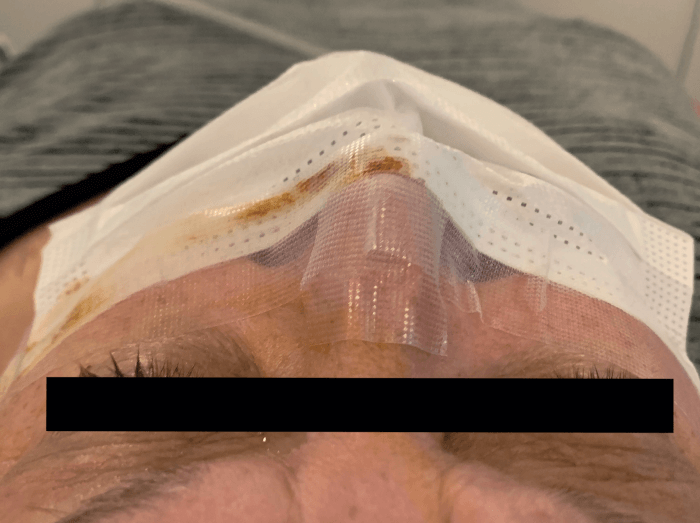
How did we mitigate that risk? We began to tape patients’ face masks along the top brim onto the midface prior to surgery (Figure 2). In so doing, we noted a significant reduction in condensation appearing on the IOL. This small, but important change has now become a standard practice at TLC Laser Eye Centers.
A simple solution
Although it is unclear whether containing air leakage from under a drape prevents any significant harm, we must protect ourselves from any factors that could potentially increase our risk of infection. Our use of IOL condensation as a marker of ophthalmic drape integrity and therefore infection transmission risk is quick, convenient, and comes at no cost. We encourage any ophthalmologist who performs IOL insertion surgery to assess the integrity of the drape seal using this technique, even if infection risk appears low. A simple adjustment to a patient’s face mask, or to your own PPE, could prevent infection.
From our experience, we suggest taping facemasks onto the patient’s midface prior to all ophthalmic surgeries as a solution to reduce air leakage; however, individual ophthalmologists may find other PPE enhancements that work more effectively or are better suited to their setting.
Our finding also highlights the importance of carefully and intentionally applying a complete seal when draping around the eye. To ensure a complete seal, we recommend taking the following steps: i) dry the patient’s skin around the eye thoroughly from any antiseptic preparation solution; ii) press firmly down on the patient’s eye for a longer duration when applying the adhesive; and iii) hold one hand down on the drape adhesive attached to the eye while using the other hand to toss the remaining portion of the drape toward the patient’s waist. Evidence has shown that a complete seal with adhesive tape around the surgical field, along with a taped facemask, can prevent the spread of respiratory droplets in cough simulation (6), so it is especially important to ensure the seal’s integrity.
We think it is vital to consider implementing these very simple steps during any IOL insertion surgery for the foreseeable future, in particular while the risk of contracting COVID-19 still exists.
Let’s not rest on laurels
With a backlog of elective surgeries, ophthalmologists may face increased pressure to complete more surgeries fast. But, considering the worldwide health and economic impacts of COVID-19, it is prudent to identify and aggressively adhere to safety precautions. Here, we have suggested a method to improve infection control measures in the OR, but concerns for future waves of infection persist. The need for vigilance in the OR is not just a personal, but also a public safety concern – so we encourage further investigation into infection control and safety measures.
Relevant disclosures: Iqbal Ike K. Ahmed has been a consultant, speaker, and received research/grant support from the following companies: Aequus, Aerie Pharmaceuticals, Akorn, Alcon, Allergan, ArcScan, Bausch Health, Beaver Visitec, Beyeonics, Camras Vision, Carl Zeiss Meditec, CorNeat Vision, ELT Sight, ElutiMed, Equinox, Genentech, Glaukos, Gore, InjectSense, iStar, Ivantis, Johnson & Johnson Vision, MicroOptx, MST Surgical, Mundipharma, New World Medical, Ocular Instruments, Ocular Therapeutix, Omega Ophthalmics, PolyActiva, Sanoculis, Santen, Science Based Health, Sight Sciences, Stroma, ViaLase, Vizzario.
The other authors have no competing interests.
References
- COVIDSurg Collaborative, “Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans: Elective surgery during the SARS-CoV-2 pandemic”, Br J Surg (2020).
- THT Lai et al., “Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong”, Graefes Arch Clin Exp Ophthalmol, 258, 1049 (2020). PMID: 32124000.
- J Liu et al., “Efficacy of slit lamp breath shields”, Am J Ophthalmol, 218, 120 (2020). PMID: 32407727.
- E Bromage, “The risks - know them - avoid them”, (2020). Available at: https://bit.ly/32XF6YP.
- C Noguchi et al., “Factors contributing to airborne particle dispersal in the operating room”, BMC Surg, 17, 78 (2017). PMID: 28683726.
- T Felfeli et al., “SARS-CoV-2 Implications in a simulated ophthalmology OR setting”, AAO (2020). Available at: https://bit.ly/2Z121Bt.
