Dry Eye Disease (DED) is one of the most common problems that we deal with in our clinics. We have seen our dry eye clinic grow exponentially as the baby boomers become older. We completed a 3 year retrospective study showing that over 75% of our dry eye disease patients were over the age of 45. These patients suffer irritation and pain due to their ocular surface disease that compels them to visit their doctor for treatment and relief. Fortunately our clinic provides many treatment modalities that can help patients improve. We also now have many tools to objectively measure severity and progress of DED. One tool that has integrated nicely into our program is the New OCULUS Keratograph 5M which is a topographer and DED analyzer. The high-resolution color camera and the integrated magnification changer offer a new perspective to the tear film assessment procedure. In this case study we will show how we use the Keratograph 5M to diagnose and follow a patient after they have had the Toyos Intense Pulse Light Treatment for Dry Eye (Dermamed).

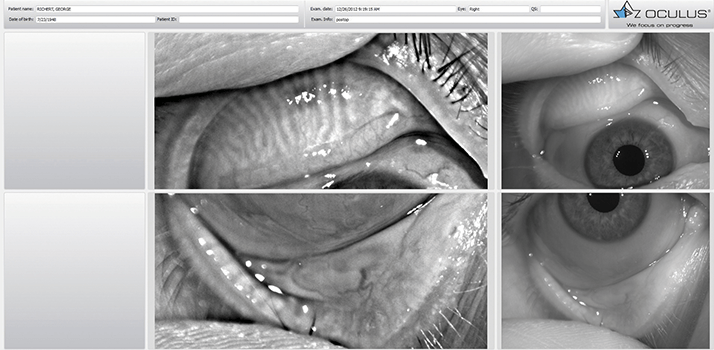
60 yr old white male complaining of red, irritated eyes for 3 years. He had been seen in several clinics where he tried 100mg doxycycline, artificial tears, restasis, warm compresses, and lid scrubs. Since we knew beforehand that the patient might be a possible dry eye evaluation when he came to our clinic we had our technician screen him using the Keratograph 5M. The first part of the screening was the Non Invasive Keratograph Break Up Time (NIKBUT). The Keratograph 5M utilizes placido ring illumination measuring thousands of points throughout the surface of the cornea. As the margins of the rings become displaced a high resolution camera records the break up in tenths of a second. A print out will show you graphically where the breakup occurred, time of the first break up, and average break up time. The advantages of using the NIKBUT is that a technician can do the scan which frees up physician time, no drops are applied to the patient‘s eyes, the results are objective and reproducible, and visual representation of the problem is available for the doctor to discuss with the patient. In this patient it is obvious that he has a poor NIKBUT making it more likely that he has Meibomian Gland Dysfunction causing evaporative dry eye.Now the technician can measure tear meniscus height which can be used as a measure of tear production. Once the patient has undergone these tests by the technician then I can begin my exam. If I determine that the patient has a poor tear film I can use the Keratograph 5M to assist me further by performing a lipid layer scan and photographing lid margin pathology. The Keratograph 5M uses white light interferometry and specular reflection to give you a colored assessment of the lipid layer. I find this lipid view reaffirms my diagnosis. All of these patients have lid margin pathology whether it is erythema, thickening of the lid, loss of lashes, scurf, scalloping of the glands, and telangiectasias. The Keratograph 5M can take a picture of this lid pathology so that you have a baseline to compare to as the patient undergoes treatment. We have found the picture and video feature invaluable in our practice not only for the clinician but as a tool to help the patient understand their disease and improvement. Here we see the patient shows all the signs of lid margin disease that accompany MGD. The next test is Meibography where an infrared light source and video camera are used on the inverted lid to show the Meibomian Glands (MG). This test is useful to record MG dropout. Studies have shown that MG dropout can lead to a poor lipid layer. We have found that lower lid drop out is more common than upper lid drop out. In a patient with evaporative dry eye poor functioning glands could be the direct cause of their DED. In this patient we see that he has some dropout in the inferior lid. http://www.oculus.de
