Perhaps you wouldn’t normally associate lymphangiogenesis with glaucoma – so why, in mice, would the deletion of genes encoding transcription factors involved in the formation of lymphatic vessels and the cardiovasculature, result in a very glaucoma-like phenotype?
A team of researchers from Illinois, Los Angeles, New York, Toronto and Uppsala were using transgenic mouse models in order to understand what role the of angiopoietin/TIE2 signaling pathway had in developing the mouse vasculature. Their model: conditional knockout mice that either have both the genes encoding angiopoetin-1 and -2 (ANGPT1 and ANGPT2) deleted after 16.5 days embryonic gestation – or the gene encoding for their receptor, TIE2 at postnatal day 0.
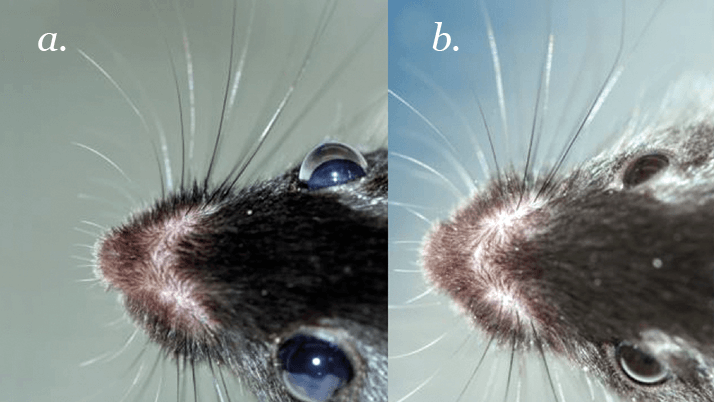
A team of researchers from Illinois, Los Angeles, New York, Toronto and Uppsala were using transgenic mouse models in order to understand what role the of angiopoietin/TIE2 signaling pathway had in developing the mouse vasculature. Their model: conditional knockout mice that either have both the genes encoding angiopoetin-1 and -2 (ANGPT1 and ANGPT2) deleted after 16.5 days embryonic gestation – or the gene encoding for their receptor, TIE2 at postnatal day 0. For their first three weeks of postnatal life, all of these transgenic mice appeared normal – indistinguishable from their wild-type littermates. But then something started to happen to their eyes. The transgenic mice started to develop elevated intraocular pressure (IOP), buphthalmos (Figure 1), and glaucoma-like features, such as retinal ganglion degeneration and vision loss – and their Schlemm’s canal was absent.
“Our finding was serendipitous,” explains one of the study’s authors, Susan Quaggin. “We were studying the angiopoietin-TIE signaling pathway, which is important for normal vascular development, and we expected to find a major effect in blood vessels. However, our studies demonstrated a key role in lymphatic vessels and particularly in the specialized lymphatic-like vessel present in the anterior chamber of the eye – Schlemm’s canal.” According to Quaggin, the disorder observed in the mice most closely resembled pediatric congenital glaucoma (PCG).
The mouse model could be a new foothold into the causative mechanisms of high IOP in glaucoma by providing the opportunity to develop and test new treatments to improve drainage of aqueous humor and prevent vision loss.
On the basis of their discovery, the researchers are now looking at developing therapies that promote lymphangiogenesis – such as angiopoietin analogs, TIE2 agonists, and even VEGF-C. “Once we identify an active drug, we need to develop a way to enhance its penetration into the anterior chamber of the eye,” says Quaggin – which suggests nanoparticle formulations.
Preclinical testing of two candidate molecules is underway, with the objective of promoting the growth of more lymphatic vessels (or enlarging existing ones) to improve drainage in the glaucomatous eye.
References
- B.R. Thomson, S. Heinen, M. Jeansson, et al., “A lymphatic defect causes ocular hypertension and glaucoma in mice”, J. Clin. Invest., Epub ahead of print (2014).
