
About your practice…
Kaweh Mansouri: As a medical and surgical glaucoma specialist, I see the full spectrum of glaucoma patients – from suspects through to advanced cases. My practice is the biggest glaucoma center in Switzerland, and we are also – in terms of output – the number one glaucoma research center in Switzerland. It is a private practice, and a teaching center.
Ziad Khoueir: BESH is a high-volume referral specialty hospital in the Middle East, and a hybrid model of private practice and teaching hospital. My practice there covers a wide range of glaucoma patients, from early glaucoma to complex referred cases of advanced glaucoma. I also cover a wide range of cataract and comprehensive ophthalmology.
How long have you been using the Kahook Dual Blade (KDB), and the new KDB Glide?
Khoueir: I’ve organized MIGS surgical wet labs with Kaweh during ESCRS meetings since 2016, featuring all the main products in the MIGS arena. At one of those sessions, Syril Dorairaj from Mayo Clinic in Jacksonville, Florida, US – an experienced KDB user – introduced me to the device. My team in Beirut performed our first cases using the KDB in 2017, and we’ve had a lot of experience with it. Earlier in 2021, we switched to the new KDB Glide.

Mansouri: I also started using the KDB thanks to Syril Dorairaj, a former co-fellow at UCSD and a good friend, who taught me how to use the device in early 2016 as one of the first specialists in Europe to try it. I started using the KDB Glide in June 2021, and have so far used it in nine cases.
What are the main features and advantages of the KDB Glide?
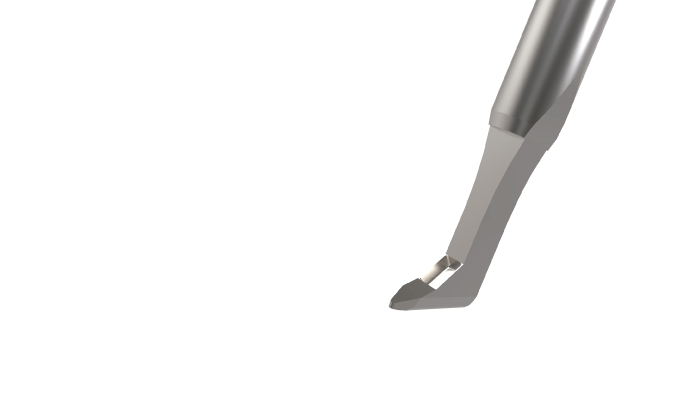
Khoueir: If I had to choose one word to describe the device, it would be: versatility. This is a highly versatile, safe and effective procedure for treating glaucoma and ocular hypertension. It’s an implant-free excisional procedure that minimizes residual trabecular meshwork (TM) leaflets. New features in the KDB Glide device reinforce these important strengths: a rounded heel, tapered sides, and smaller footplate deliver optimal interface with Schlemm’s canal, permitting precise excision with the instrument’s proprietary dual blades, even in variable anatomy.
Mansouri: The KDB Glide shows that New World Medical listens to surgeons. This new, updated version of the original KDB has not just been brought out to keep people interested in the technology – it has been based on genuine, important feedback from us, the users. The main design change eases the movement of the footplate in Schlemm’s canal, and allows for anatomical variations among patients.
Not every canal of Schlemm is the same – they differ in size, curvature, obstructions, and all these differences have an impact on the procedure. In the KDB Glide, the foot is more rounded than in the original KDB, and it enables the device to even better conform to Schlemm’s canal. Moreover, the bottom edge of the device is tapered, which reduces resistance, and creates less friction with the anterior wall of Schlemm’s canal.

Which patients do you recommend this tool for?
Mansouri: As with the original KDB, I use it for early to moderate glaucoma patients – those who don’t necessarily need an IOP lowering, but would like to reduce the number of medications, and those who need a reduction in both the IOP (to midteens) and the number of medications. I like to use it for combined surgery, if needed. In angle closure patients, especially those with peripheral anterior synechia, I can use the KDB Glide and perform Goniosynechialysis (GSL) and open the angle, before continuing to Schlemm’s canal. It’s a big, unique advantage of the device; no other MIGS device can be used in angle closure.
Khoueir: The KDB Glide is ideal for cooperative patients who will benefit from enhanced outflow of aqueous. Preoperative gonioscopy is crucial in-patient selection. I need a good view on gonioscopy with clear anatomy and ideally a pigmented nasal TM. I’m currently using it either as a combined procedure with phaco or as a standalone treatment at any stage of glaucoma from early to severe, including secondary open angle glaucoma. Combining it with phaco and GSL has also become my procedure of choice in most primary angle closure glaucoma cases. Being able to offer excisional goniotomy in my practice allowed me to be more proactive in early and moderate glaucoma. It is also a suitable and effective option in many cases of advanced disease where I feel my hands are tied, and where I want to reach the target with a minimally invasive approach.
What outcomes have you been able to achieve with the KDB Glide?
Khoueir: My team’s two-year data with the first iteration of the KDB shows a significant average IOP reduction of 27 percent, and a 50 percent reduction in the number of glaucoma medications when combined with phaco. Our patients are happy and grateful to have better IOP control and to be less dependent on their medications.
Mansouri: I haven’t collected enough data on KDB Glide yet to be able to give a definite answer, but – after only two or three months – I can say that clinical results are as good as with the original device. The reduced friction might result in less scarring and better outcomes – it’s too early to say – but the KDB Glide is certainly easier for surgeons to use.

Your tips for surgeons using the device for the first time?
Mansouri: As I mentioned, the KDB Glide is easier to use than the previous generation of the KDB so I think most existing KDB users will appreciate it even more. For those who haven’t used the KDB yet, I would recommend they go straight to the KDB Glide – it is even more user friendly. You should be comfortable with gonioscopy, so if you are – just go for it!
Khoueir: My experience with the first generation was really good and the learning curve was quite straightforward. The procedure is quite intuitive – the most intuitive procedure in its category – and it’s rewarding to be able to see anatomically how you are removing a strip of TM.
The new KDB Glide makes it even easier for surgeons who are new to angle surgery. Cataract surgeons who don’t have experience with angle surgery should not feel intimidated and simply try it; a good way to start is by practicing gonioscopy in the clinic and in the OR on regular cataract cases. Trypan blue stains the trabecular meshwork (TM), which helps with first cases. Patient selection is very important, and you might be better off starting with patients who have a well pigmented angle nasally. Last but not least: patient education and counseling about the risks and benefits of the surgery are key. Patients need to understand what the procedure is about, and their expectations should be realistically aligned with what MIGS can offer.
Any final thoughts?
Khoueir: I find the KDB Glide to be quite effective and safe. The most frequent postoperative “complication” that you should expect is hyphema in around 20-30 percent of the patients. The vast majority of those cases are self-resolved and only require conservative management. I always discuss hyphema with my patients before the surgery and tell them that they should expect it because we are “unclogging the drain.” This reassures them if they have some blurred vision early postop. During surgery, blood reflux is a good prognostic sign, indicating patency of the outflow system, and should not be perceived as a complication of the procedure.
Mansouri: The results of the KDB speak for themselves. For me, it’s probably best-in-class in its category. It is also the most economical, cheapest device I use, which is a very important consideration especially for developing countries. It makes it likely the only affordable MIGS device for low-income locations, and I know that New World Medical have made a real effort to keep the price as low as possible for this reason. It opens up the indication for resource-poor regions, and – importantly – for closed angle glaucoma.
