

- Anti-VEGF therapy is the current gold-standard for treatment of wet AMD
- A plethora of approaches offer promise of effective adjunctive therapies
- Stereotactic radiation prevents growth of abnormal blood vessels
- Single treatment reduces the need for on-going anti-VEGF injections
In his 17th century stone house in Norfolk, England, Jonny Gathorne-Hardy surrounds himself with tomes of all kinds, especially reference books, biographies and histories. Some he penned himself, and others hold valuable insights that will enrich his next work. It is here, often in front of a gas fire or wood stove, that Gathorne-Hardy will write hundreds of words a day, polishing his prose well into the night. He is a renowned and versatile author, and many of his children's books, novels, short stories and plays have been published.
Wet AMD is the leading cause of blindness in people over 65 in the Western world. In the UK, for example, it affects approximately 260,000 people, and approximately 40,000 new cases are diagnosed each year. Often, early wet AMD is asymptomatic. Patients who do display symptoms may notice sudden loss of central vision, deterioration of visual acuity, optical distortions, or blind spots.
Evolving Therapeutic Strategies
What must the medical community do to reach the elderly population with the urgency and frequency demanded of wet AMD? Early diagnosis can not only save vision, it can also expand the treatment options available to those whose sight is threatened.The excitement around anti-vascular endothelial growth factor (anti-VEGF) drugs is well justified. Medications such as ranibizumab (Lucentis), pegaptanib (Macugen), and bevacizumab (Avastin) have completely changed the treatment paradigm for wet AMD, saving vision in what previously would have been nearly hopeless situations. Aflibercept’s (Eyelea) benefits of less frequent dosing and potential efficacy for those who are resistant to other anti-VEGF treatments are also a welcome development.
Yet for all their value, anti-VEGF drugs have significant limitations. Research shows that they are most effective when administered frequently (1). This translates into regular eye injections, as this is how anti-VEGF therapies are delivered; understandably, many patients do not relish the thought of this. In addition, receiving these therapies results in considerable inconvenience to patients and their families, like traveling to distant locations for both injections and post-treatment follow-up. Consequently, many patients drop out of therapy after a year or two, and incur the substantial risk of progressive visual loss. Despite this, it’s not uncommon for medical staff to work long hours to accommodate the volume of anti-VEGF injections that need to be administered; this will only continue to increase as the baby boomers age. Additionally, this represents an enormous cost burden to healthcare systems that must support an indefinite commitment to expensive and frequent therapy.
Anti-VEGF injections are the current gold standard for treating neovascular AMD, but adjunctive therapies with other drugs or treatment modalities are garnering increasing interest. Stereotactic radiation therapy is already commercially available in Europe, and the pipeline of investigational treatments worldwide is burgeoning: pills, eye drops, sustained-release delivery systems and stem cell therapies are among the innovations under development.
As these new approaches emerge, they raise important questions for clinical management. Who is best suited for monotherapy? Which patients can benefit most from adjunctive therapy? At what point will it be necessary to identify candidates for additional therapies? How will the best responders for these new therapies be identified?
Many patients do well with anti-VEGF injections but the treatment burden and costs are significant. Alternative therapies offer one means to address this critical need. While such treatments may or may not eliminate the need for anti-VEGF injections entirely, they may at least reduce their frequency, lessening the inconvenience to patients and the cost burdens on the health care system.
Stereotactic radiation
Radiation has a long history in the treatment of cancer. It is very effective in the destruction of rapidly dividing tumor and vascular cells. Unlike ablative therapies, such as laser photocoagulation that burn tissue and often cause permanent scarring, ionizing radiation disrupts cell division by affecting DNA repair mechanisms. Cells undergoing rapid growth are more radiosensitive than senescent or slowly-dividing cells, so ionizing radiation is used medically for its anti-angiogenic, anti-inflammatory, and anti-fibrotic effects, which likely play a role in its impact on wet AMD (2).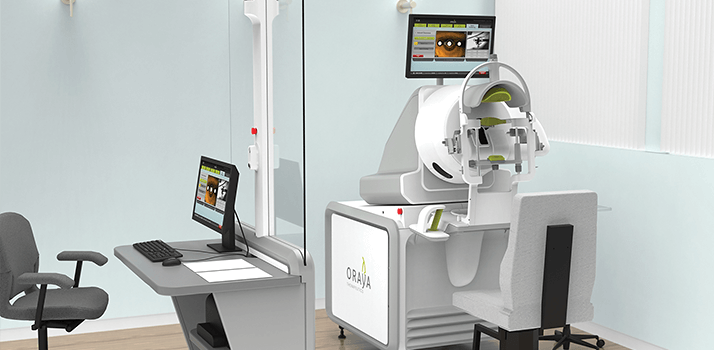
(Bottom) Mr. Gathorne-Hardy positioned in the IRay System.Oraya Therapy (see Figure 1), developed by Oraya Therapeutics, Inc., is the stereotactic delivery of low-voltage X-rays for the treatment of AMD-related choroidal neovascularisation. The Oraya device uses a proprietary narrow, low-energy (100 kVp) X-ray beam to treat a small volume of the retina at the macula. The X-ray beam is incident onto an integrated beam-stop, so scattered radiation levels are ? very low, meaning that additional shielding is unnecessary. The highly collimated beams, 4 mm in diameter, allow precise targeting of the macula while minimizing dose exposure to other tissues. The patient total-body effective dose is comparable to a head radiography series, or one-tenth of a head CT scan. The entire procedure takes about 20 minutes and the patient can go home after appropriate post-treatment evaluations are made.

Gathorne-Hardy was first diagnosed with neovascular AMD in his left eye in 2008 and received ongoing ranibizumab injections. Unfortunately, he gradually lost vision. Then his right eye developed the disease in June 2010. In part, because the condition in his right eye was identified early, he was considered to be a prime candidate for treatment with stereotactic radiation, and was enrolled in the INTREPID clinical trial, a study that evaluated Oraya Therapy as an adjunct to anti-VEGF injections that was performed at King’s College Hospital, London, in August 2010.
After treatment, Gathorne-Hardy’s visual acuity in the right eye significantly improved, with a nine-letter gain, even without any subsequent injections into the eye or any other treatment. More than two years later, he continues to enjoy a seven-letter improvement. With the subsequent commercial availability in the United Kingdom, Gathorne-Hardy is now keen to see if the Oraya Therapy can be used on his other eye, which has been badly affected by wet AMD and requires continued injections.
In the INTREPID study, which enrolled a wet AMD patient population previously treated with anti-VEGF for up to three years, the Oraya Therapy group experienced a 32 percent reduction in the number of injections and had substantially drier retinas compared with controls who did not receive radiation (2). Additionally, 25 percent of the Oraya Therapy patients needed no further injections during the first year of follow-up, and the mean visual acuity of this group was maintained compared with controls, even though significantly fewer injections were administered. A well-defined subgroup of patients that has lesions that fitted within the X-ray beam spot, and also exhibited significant macular fluid, achieved a 55 percent reduction in injections with over a line of vision superiority compared with the subgroup controls. This group of patients is estimated to represent over 60 percent of the wet AMD patient population.
This is an exciting time for the treatment of wet AMD. As more therapies come onto the market, their integration into practice patterns and interpretation of new research findings will present challenges. It’s a nice problem to have, and patients will reap the benefits.
E. Mark Shusterman is the Medical Director for Oraya Therapeutics.
Videos
- orayainc.com/oraya-therapeutics/
- orayainc.com/about-oraya-therapy/video/
- orayainc.com/patients/resources/
References
- D. F. Martin et al., “Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results”, Ophthalmology, 119, 1388-1398 (2012). T. L. Jackson et al., “Stereotactic Radiotherapy for Neovascular Age-Related Macular Degeneration: 52-Week Safety and Efficacy Results of the INTREPID Study,” Ophthalmology, 120, 1893-900 (2013).
