For years, dry eye specialists have encountered patients whose symptom severity is conspicuously worse in the morning. In response, we developed practical tips to help patients avoid desiccating stresses at night. These recommendations frequently involve instructing the patient to avoid turbulent air across the faces (fans, AC, forced air heat), allergens and mites. Many of these patients follow our instructions diligently and still wake up dry, inflamed and in pain. Fortunately, in recent years, we’ve gained important insight into several of the underlying mechanisms contributing to this problem. We have subsequently identified nocturnal lagophthalmos – or insufficient eyelid seal – as a more prevalent and influential compounding factor than previously believed.
Adjusting the algorithms
Recent research establishes that compromised lid seal – a condition wherein a patient’s eye lids remain partially open during sleep – potentially affects up to 79 percent of all symptomatic dry eye patients across diverse demographic groups (1). Interestingly, patients with asymptomatic dry eye show comparatively and significantly less lid seal failure, and the severity of a patient’s lid performance failure correlates heavily to the degree of dry eye symptom severity observed. Given this understanding, it is crucially important that we adjust our diagnostic algorithms to identify dry eye and MGD patients with poor lid functionality – those patients who are particularly susceptible to nocturnal lagophthalmos. For these patients, avoiding fans, allergens and other commonplace aggravators simply isn’t adequate. When the eyelids’ protective biomechanics are insufficient, they leave the ocular surface exposed at night, and desiccating stress is inevitable without a more specific and robust treatment strategy. Proactively addressing this problem is important, as desiccating stress is a known trigger for chronic inflammation leading to chronic dry eye disease (2).
Lid light leakage
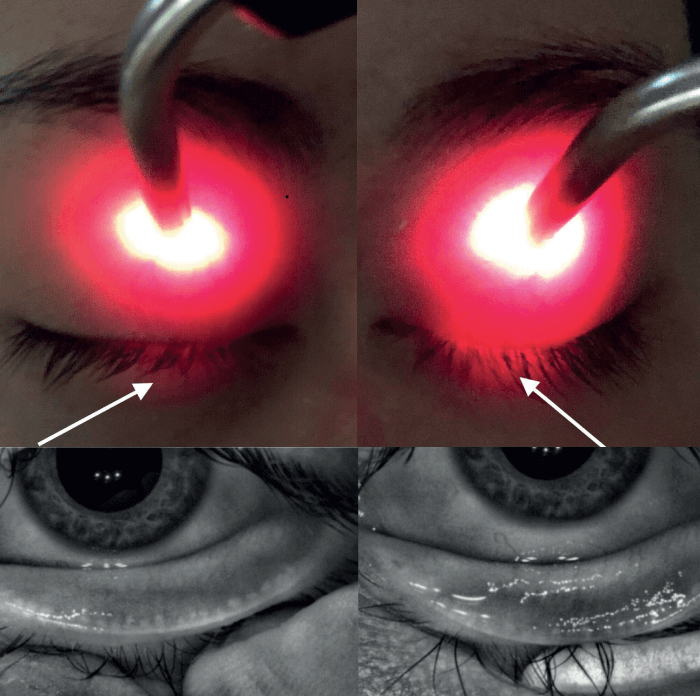
The “Korb-Blackie Lid Leak Test” is a simple and effective way to identify dry eye and MGD patients with insufficient lid seal (3). The test can be carried out in any exam room with basic equipment. In a dark room, gently place a muscle light or transilluminator at the upper tarsus of a closed eye and direct the light toward the interpalpebral fissure. If light escapes between the eyelids, the patient’s lid seal is inadequate. The more light that “escapes” the interpalpebral fissure, the higher degree of dysfunction and greater exposure to desiccating stress at night (see Figure 1). In our practice, we record this in the EMR as “lid seal insufficiency,” grading the condition negative, mild, moderate or severe based on the amount of light leakage.
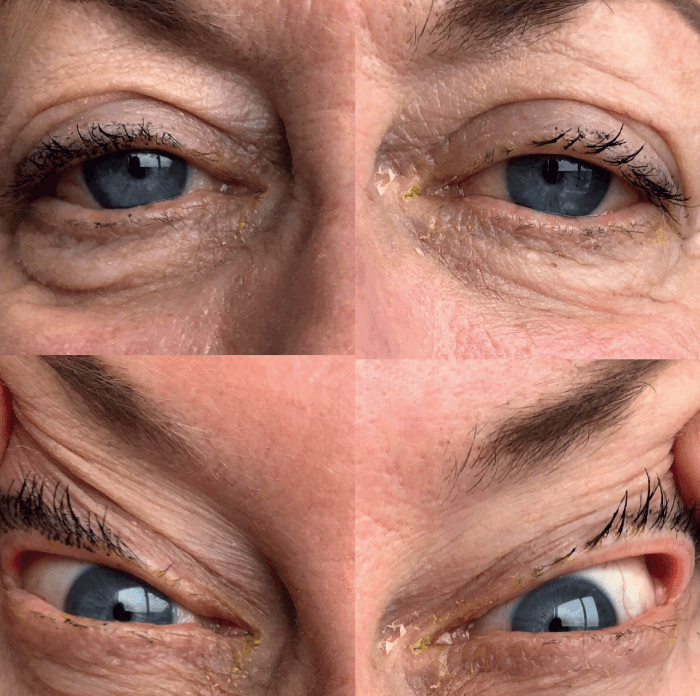
We can also use a simple and effective “snap test” to manually assess a patient’s lid position. A snap test is performed by gently pulling the patient’s upper and lower eyelids away from the globe in a pinch like fashion then releasing. Lids that snap into place quickly are elastic and likely healthy, while lids that are slow to normalize may indicate excess laxity, functional lid malpositions, abnormal lid wiper mechanics and potentially, insufficient nocturnal lid seal. We pull on the upper lid superiorly and temporally from the globe (see Figure 2). Excessive amounts of upper lid laxity and distractibility from the globe are highly suggestive of floppy eyelid syndrome (FES). In these patients, we order a sleep study to identify obstructive sleep apnea (OSA), which is often associated with FES (5). In severe cases of FES, surgical repair may be required (6).
The pathophysiology of FES is interesting and multifactorial. Recent research suggests that floppy eyelids are associated with physical influences introduced over time: specifically, sleeping preferences – even face-down may exert tractional forces on the eyelid(s) (7). Ischemic damage is well described in obstructive sleep apnea and is associated with chronic inflammation. Additionally, a post-surgical FES repair tissue analysis series demonstrated very high amounts of metalloproteinases in the tissues. One common theory is that the hypoxic episodes associated with obstructive sleep apnea create a smoldering inflammation which, over time, destroys the elastin fibers (8) and collagen fibers of the eyelids thereby creating the lid laxity, lash ptosis, and papillary conjunctivitis characteristic of FES (9). Treatment of OSA with CPAP has been reported to result in improvements in FES (10) and this is consistent with our clinical observations.
Controlling the cascade
If a patient’s lid seal insufficiency and dry eye signs/symptoms are mild, I may advise them to use preservative-free OTC lubricating gels and ointments. However, for patients with moderate or severe signs and symptoms, I use a silicone medical-grade vaulted sleep mask developed for dry eye and MGD patients (such as eyeseals, Eye Eco), and specially designed to work with CPAP devices. By creating a comfortable seal around the periocular region, moist protection of the ocular surface is recreated. My patients report that the mask helps them sleep better and that their morning symptom severity is reduced. Some MGD patients report improved symptoms with night mask wear particularly if there is a component of allergy to dust mites. Clean the masks every morning in a simple soap that is free of perfumes, triclosan and colorants (such as diluted Dr Bronner’s soap). In the MGD cases with excessive lid laxity, we have clinically observed that customizable thermal expression modalities, such as TearCare or iLux, provide a therapeutic advantage as the LipiFlow activators can be less likely to remain in optimal position on lax eyelids during treatment.
With the abundance of diagnostic and treatment strategies, we are able to reduce or prevent the desiccating stress-induced chronic inflammation cascade that characterizes dry eye. It is only by recognizing and minimizing the impact of nocturnal lagophthalmos that a protective ocular surface environment can be recreated – one that reduces symptom severity and helps our broad range of prescription, nutrition supplemental, and in-office treatment modalities work more effectively.
Disclosures: Laura Periman is a speaker for Allergan, Lumenis, Novartis and Sun Pharmaceuticals. She also serves as a consultant for Alcon, Eyedetec, Eyevance, Science Based Health, Sight Sciences, TearLab and Visant.
References
- D Korb et al., “Prevalence of Compromised Lid Seal in Symptomatic Refractory Dry Eye Patients and Asymptomatic Patients”, Invest Ophthalmol Vis Sci, 58, 2696 (2017).
- J Craig et al., “TFOS DEWS II Definition and Classification Report”, Ocul Surf, 15, 276 (2017). PMID: 28736335.
- D Korb and C Blackie, “The Korb-Blackie Lid Light Test”, Invest Ophthalmol Vis Sci, 54, 942 (2013). PMID: 25503913.
- D Liu et al., “Tear Film Dynamics in Floppy Eyelid Syndrome”, Investigative Ophthalmology & Visual Science, 46, 1188 (2005). PMID: 15790878.
- A McNabb, “The eye and sleep apnea”, Sleep Med Rev, 11, 269 (2017).
- L Periman and B Sires, “Floppy eyelid syndrome: a modified surgical technique”, Ophthalmic Plast Reconstr Surg, 18, 370 (2002). PMID: 12352824.
- M Sward et al., “Lax Eyelid Syndrome (LES), Obstructive Sleep Apnea (OSA), and Ocular Surface Inflammation”, Ocul Surf, 16, 331 (2018). PMID: 29729418.
- P Netland et al., “Histopathologic features of the floppy eyelid syndrome. Involvement of tarsal elastin”, Ophthalmology, 101, 174 (1994). PMID: 8302552.
- A McNab, “Reversal of floppy eyelid syndrome with treatment of obstructive sleep apnea”, Clin Exp Ophthalmol, 28, 125 (2002). PMID: 10933776.
- O Idowu et al., “Floppy eyelid syndrome: ocular and systemic associations”, Curr Opin Ophthalmol, 30, 513 (2019). PMID: 31483320.
