“How does my eye look? Is it getting worse?” Those were the questions asked by a patient during my cornea fellowship many years ago. I reviewed the scanned hand-written notes and, unable to tell if she was getting better or worse, I typed out as many descriptive words I could think of into the EMR computer. I swallowed, took a deep breath, and asked the patient to wait for my attending surgeon to deliver the news.
What’s surprising is that this scenario of hand-written notes in paper or electronic medical records still happens in the 21st century. “There’s absolutely no way you can remember. You have to take eye pictures and compare,” my fellowship mentor at the University of California, Los Angeles, Dr. Bart Mondino, told me as he pulled out some Kodachrome slide photos of the patient’s eye from past visits. Thinking back, he was absolutely correct and taught me an extremely important lesson.
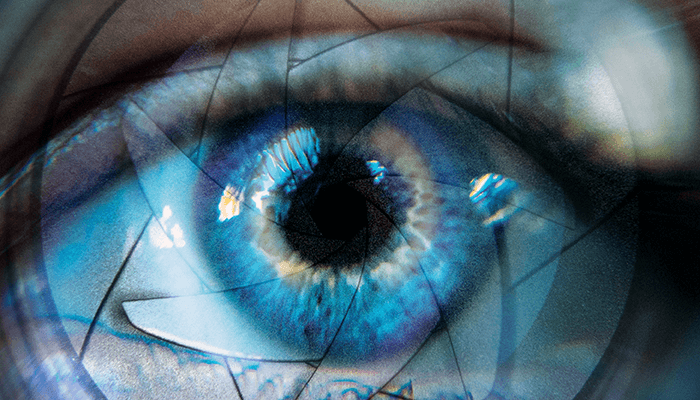
Taking photos of your patients’ eyes as an ophthalmologist should be an important part of any clinical practice. Creating detailed drawings, recording copious notes, or grading various eye conditions cannot compare with the information one receives from viewing a crisp, tack-sharp photo of an eye. In my career, I’ve conducted at least 150,000 patient eye exams, and there is no way I can remember every single eye and how it appeared in the past – no doctor can! Taking these photos has many benefits for both ophthalmologists and patients. The obvious reason is to track progress. As I see the same patient over time, I can compare their eye photos and monitor their condition if it gets better or worse (this goes for myriad conditions but includes cataract progression, conjunctival pigmented lesions, healing corneal abrasions/ulcers). This helps me be a better ophthalmologist and it allows for quicker follow-up visits and better patient satisfaction – because the patient is an active participant in their care. They can see what’s going on instead of just processing their diagnosis. The words I often hear from patients after I show them their eye photo are – “Wow!” or “I get it now!”
A digital boon?
Back in the beginning of the 21st century – just before the dawn of the digital photography revolution – it was easier for my mentor, working at an academic institution, to take a photo of every patient because of the available resources: a dedicated ophthalmic photographer, a photo processing lab, and plenty of space to store hard-copy Kodachrome slides of patient eye photographs. Joining a private clinical practice (with no residents/fellows to help) and taking a photo of every patient’s eye was just not practical from an economic and workflow standpoint. Slit-lamp mounted cameras were expensive and there was no way to justify the ROI when reimbursement for eye photos was so low. Thus, with the surge in popularity and the steadily declining costs of digital SLR cameras in the 2000s, I began to take digital photos of my patients' eyes using a heavy DSLR camera with a large macro lens.
When used in front of a patient’s eye, it was intimidating – like looking down the barrel of a gun. There were other friction points too; I had to take pictures of the patient’s eye using the camera, then take the SD digital card out and upload it to the slow hospital EMR computer. This took a lot of time and wasn't feasible for every patient. As the years passed, I migrated to a point-and-shoot digital camera that I mounted to a slit lamp with an expensive adapter. This was less intimidating for the patient, but the photo quality wasn’t very good – and I still had to manually take the SD digital card out of the camera and upload it to the slow, clunky hospital EMR computer.
The smarter revolution: large screen phones with better cameras
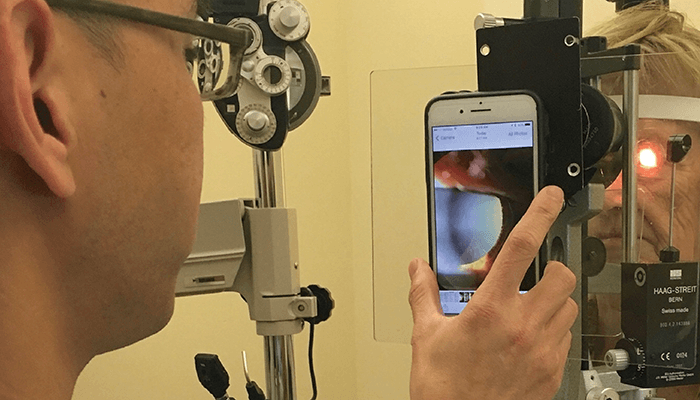
The key moment for me as an ophthalmic photographer was the introduction of the iPhone 6 Plus in 2014. The combination of the iPhone’s large screen, improved camera sensors, fast Wi-Fi connectivity, and a growing ecosystem of mobile electronic medical record (EMR) apps started to redefine what a smartphone could do for an ophthalmologist. Our team began to tinker and develop a custom mount for the iPhone 6 Plus to connect it with the slit lamp I normally used.
The larger iPhone screen size meant that I no longer had to upload photos via an SD card to a nearby hospital or office PC; I could take the photo and show it to the patient instantly. The birth of EMR imaging apps shortly after the debut of the iPhone 6 Plus also meant that I could upload the patient’s eye photo into their record within seconds – another time-saving point for a busy ophthalmologist. Certainly, these photos are important for the me as a clinician – but they could also help other clinicians, who may treat the same patient in the future, by allowing continuity of care. For me, the iPhone essentially became a portable camera with a fast computer attached to it.
Patients often face difficulty accessing eye photos when they travel, move, or have to engage with another healthcare system. I developed the idea of using Apple’s AirDrop feature to wirelessly send these photos straight to the patient’s iPhone, allowing them to access it whenever it was needed. For Android users, I send the photos via Doximity Dialer using a HIPAA secure text with attachments, while safeguarding my phone number. This ensures the patient’s eye photo stays with the patient – not with a potentially hackable or misused cloud EMR server.
Smartphone macro eye photography and telehealth
The introduction of the iPhone 13 Pro was also another key moment for ophthalmic photography. A pro-level camera was now available on a smartphone that was connected to an ultra-fast 5G connected miniature computer in your pocket. For the first time ever, it was possible (with proper lighting) to take a high-definition macro image of the eye without the need for an expensive slit-lamp.
I posted this feature on LinkedIn and immediately faced criticism from macro-photographers all over the world. They were missing the point. It wasn’t about me as an ophthalmologist taking great smartphone eye photos. It was about everyone else in the world now having the ability to do so.
Imagine the potential for improved access to expert eye care for patients in remote areas of the world – all thanks to the ability to take a photo of their own eye and send it digitally to an ophthalmologist via telehealth. This truly revolutionary step forward in healthcare could empower patients to get the care they need without having to travel. And it could have an immensely positive impact on the lives of people who would otherwise be unable to get access to expert ophthalmic care.
Embrace the eye photo
The future of visible light eye photography is incredibly exciting. With the rapid advances in smartphone camera and telehealth technologies, we are able to provide previously unseen levels of in-person and remote ophthalmic healthcare. It has never been easier to take digital eye photos, and, with the right knowledge and guidance, it can empower your patients.
As a practicing clinician, you have the power to collaborate and innovate in ophthalmology. With a digital eye picture you can say so much more than a thousand words – so, go take some photos and see what you can discover!

