
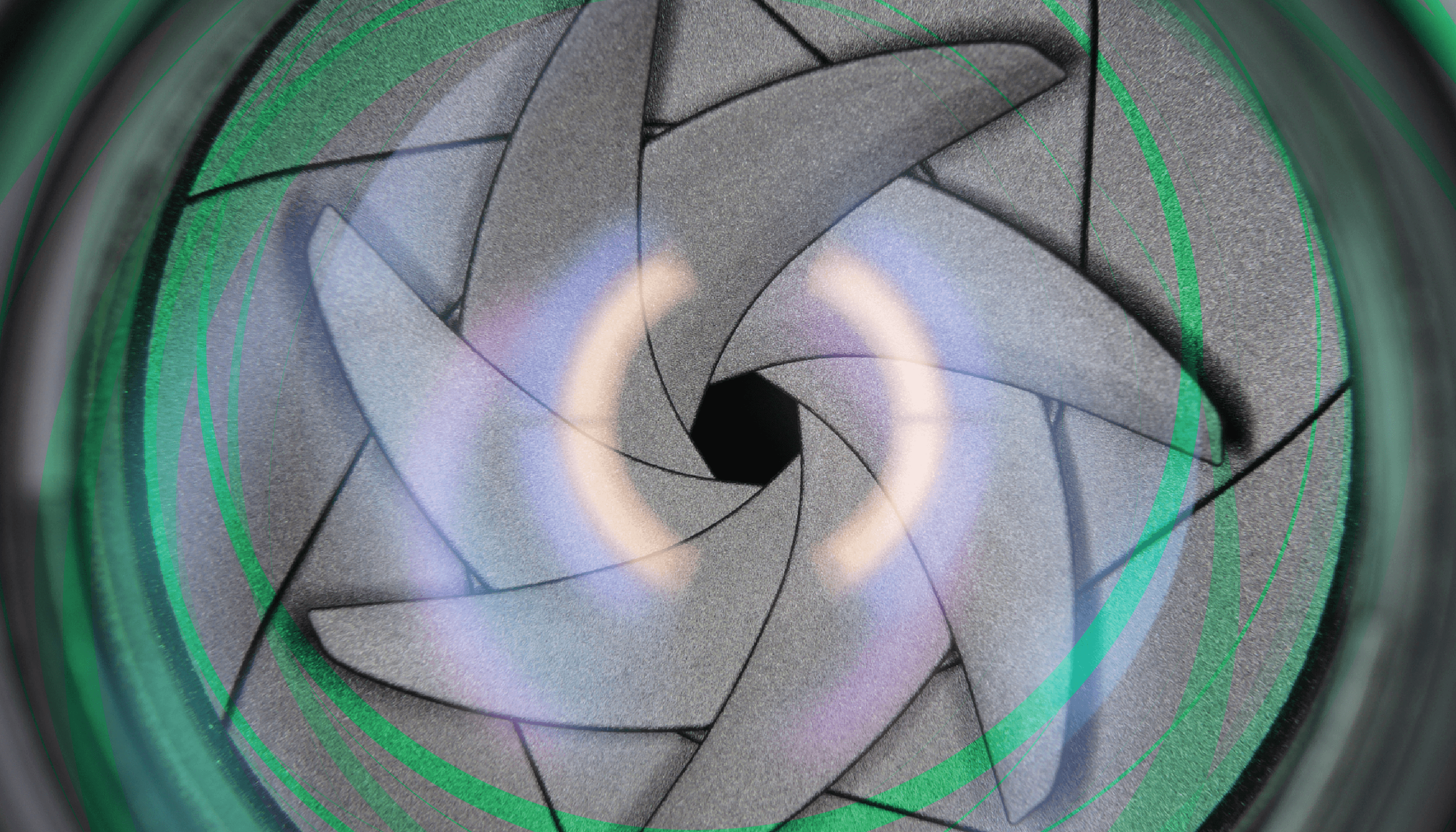
Pupil-modulating presbyopia drops rely primarily on the principle of pinhole optics. Channeling light through a smaller central aperture, created pharmacologically in this case, sharpens vision under most lighting conditions and increases the depth of focus. Pinhole optics have already been leveraged, with good refractive results, for implanted devices in the form of corneal inlays and small-aperture IOLs. Now, with the introduction of VUITY and several other miotic-based presbyopia-correcting drops, pinhole optics may prove to be an ideal solution for some of the common postoperative problems we encounter as cataract surgeons.
New and upcoming drops modulate the pupil using familiar agents such as pilocarpine, carbachol, and brimonidine. Although these agents have long been available in some form, they were not practical for daily presbyopia correction. New formulations have been optimized using lower concentrations of the active ingredients and advanced vehicles expected to offer better penetration, more comfortable instillation, and reduced side effects. VUITY drops contain a low concentration of pilocarpine and were designed to quickly adjust to physiologic pH to improve tolerability of the acidic active ingredient. A fixed-combination preparation from Visus Therapeutics (BRIMOCHOL PF) includes the sympatholytic alpha-2 agonist, brimonidine to inhibit contraction of the iris dilator muscle, potentially reducing ocular surface redness due to the vasoconstrictive effects of brimonidine on the conjunctival vessels. Nonclinical studies have also indicated that brimonidine may reduce ciliary body contraction and markedly increase carbachol bioavailability, resulting in increased duration over carbachol monotherapy.
A better range of vision
The largest group of pseudophakic patients potentially set to benefit from drops are those who have already had cataract surgery with a monofocal IOL. Offering these patients topical drops to temporarily improve their near vision could be a significant lifestyle enhancer.
The evidence from FDA trials of surgical small-aperture technologies suggests pinhole optics preserve patients’ distance acuity (1, 2). In ongoing clinical trials for presbyopia-correcting drops, the FDA is requiring manufacturers to demonstrate that products can achieve near vision gains with less than one line loss of distance vision. This provides confidence in trying these drops in pseudophakes who already have good distance vision but desire a more functional range of vision for all or part of their day.
Addressing residual error
Predictably, many of our pseudophakic patients don’t have great uncorrected near or distance vision. For patients who still need to wear distance correction after cataract surgery, presbyopia-correcting drops could offer the option of wearing single-vision glasses, especially in unfamiliar environments, and being less dependent on bifocals or progressive spectacles. Spectacle multifocality creates blur on the downgaze and impairs edge-contrast sensitivity and depth perception, increasing the risk of falls (3).
Presbyopia-correcting drops may also help patients with up to 1.5 D of residual astigmatism see better (2, 4). By blocking aberrated peripheral light rays, pinhole optics improve astigmatism tolerance. In patients wearing glasses primarily for astigmatism and near vision, this effect could provide less spectacle dependence during the work day or for social activities.
Dealing with dysphotopsia and aberrations
We know from looking at modular transfer function graphs that visual quality is always better with narrower pupils. The pinhole effect of blocking stray light and unfocused peripheral light has added benefits of minimizing not only regular astigmatism and defocus, but also the impact of irregular corneal aberrations on vision. We have post-Radial Keratotomy patients whose incisions have caused hyperopic shift and fluctuating vision throughout the day. A smaller pupil makes them less sensitive to those fluctuations. I believe such patients will ultimately benefit the most from a small-aperture IOL. In the meantime, presbyopia-correcting drops give them a chance to test out pinhole optics in advance and perhaps carry them through for a few years before they are ready for lens surgery.
We also have patients in our practices who received early presbyopia-correcting IOLs with a high add power, which typically provided excellent near vision but with more dysphotopsia at night. While some patients neuroadapted to them, others found the glare and halo disabling at night and have had to restrict night driving. I have sometimes treated these patients with topical brimonidine because of its action in preventing pupillary dilation which, in a presbyopia drop, is complementary to constricting the pupil. Should drops like BRIMOCHOL PF be approved in the future, a drop in the non-dominant eye at nighttime may also help to prevent defocus-related glare and halo from the IOL in patients whose primary issue is dysphotopsia.
Prescribing considerations in pseudophakes
So far, presbyopia-correcting drops have only been tested in pseudophakes in a few clinical trials, and clinical experience with VUITY, at the time of this writing, is still limited. There are still questions to be answered about how well these drops will work for a pseudophakic population. My hope is that pupil modulating drops will work well bilaterally, without any loss of distance acuity or significant dimness. A 2019 review of small-aperture strategies for presbyopia reported that perceived brightness through a small aperture is greater than what would be expected from theoretical calculations (5). However, we still want to monitor how well new presbyopia-correcting drops perform in dim light.
We may want to exercise caution in prescribing the drops for patients who already have reduced contrast sensitivity from optic neuropathy or macular degeneration. It may become more important to get a baseline pupil size in patients, especially if they are elderly or on medications that already tend to affect pupil size. These patients might not respond to miotics for presbyopia at all, or may be more challenged by dim light. Additionally, just as with presbyopia-correcting IOLs, it will be important to appropriately manage the ocular surface. Pinhole optics won’t work very well if the patient has superficial punctate keratitis in the center of the pinhole. Importantly, it is prudent to perform a dilated fundus exam and discuss the risk of retinal complications that miotics may exacerbate in some at risk eyes.
There will likely be some variability in effectiveness, due to refractive status, age, or other patient factors we don’t yet fully understand. However, unlike IOLs or corneal inlays, patient response isn’t necessarily a cause for immediate concern. If one particular drop doesn’t work, patients can stop using it or wait for one with a better side effect profile or longer duration of effect to hit the market. This new category is full of promise, both for routine correction of presbyopia and for resolving tough postoperative problems.
 Credit: D-Kuru from Wikimedia Commons
Credit: D-Kuru from Wikimedia Commons
References
- JA Vukich et al., “Evaluation of the small-aperture intracorneal inlay: three-year results from the cohort of the U.S. Food and Drug Administration clinical trial,” J Cataract Refract Surg, 44, 541 (2018). PMID: 29759685.
- HB Dick et al., “Prospective multicenter trial of a small-aperture intraocular lens in cataract surgery,” J Cataract Refract Surg, 43, 956 (2017). PMID: 28823444.
- SR Lord et al., “Multifocal glasses impair edge-contrast sensitivity and depth perception and increase the risk of falls in older people,” J Am Geriatr Soc, 50, 1750 (2002). PMID: 12410892.
- AE Ang, “Small-aperture intraocular lens tolerance to induced astigmatism,” Clin Ophthalmol, 12, 1659 (2018). PMID: 30233128.
- HB Dick, “Small-aperture strategies for the correction of presbyopia,” Curr Opin Ophthalmol, 30, 236 (2019). PMID: 31033734.
