- Anti-VEGF agents have revolutionized the treatment of the choroidal neovascularization that’s present in so many retinal disorders, such as AMD, DME and branch and central RVOs
- Administration typically involves regular, monthly, transscleral injections of the drug into the posterior chamber via an intravitreal approach – for the remainder of the patient’s life
- A new method of injection has been developed, whereby in pseudophakic patients, a perilimbic approach is used instead
- This technique could avoid several of the complications associated with transscleral intravitreal injections and can be employed by ophthalmologists who aren’t retina specialists
The introduction of vascular endothelial growth factor (VEGF) inhibitors has revolutionized the treatment of many retinal disorders: wet age-related macular degeneration (AMD), diabetic macular edema (DME), and macular edema secondary to central or branch retinal vein occlusions. However, that treatment comes at a cost: monthly intravitreal injections by a retinal specialist for the rest of that patient’s life.
The standard approach involves injection of approximately 50 μL of drug (in this case, bevacizumab) solution via a needle inserted through the pre-anesthetized conjunctiva and sclera, placing the needle approximately 3.5–4.0 mm posterior to the limbus, while avoiding the horizontal meridian and aiming toward the center of the globe. The injection volume is delivered slowly and the needle removed slowly to ensure that all solution has been injected (see Figure 1). Complications are rare – but they tend to be serious, and include retinal detachment, retinal pigment epithelial laceration and retinal hemorrhage – among others.
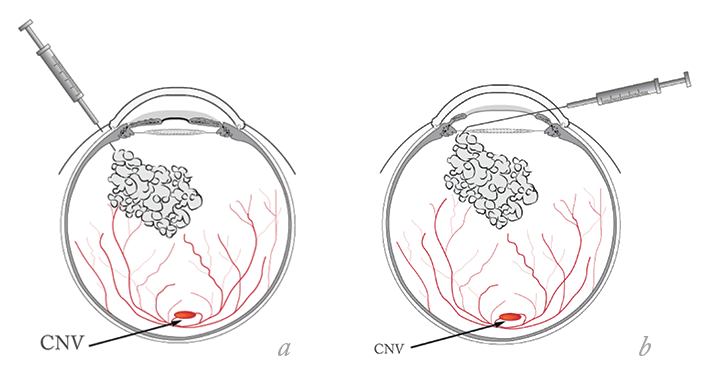
To avoid some of the adverse complications associated with intravitreal drug delivery, we have developed a novel technique to deliver VEGF inhibitor therapy into the posterior chamber in pseudophakic eyes. Crucially, our method (see Box) avoids contact with the sclera or retina. By accessing the posterior chamber using the perilimbic route, we avoid injury to the sclera and the retina, although possibility of corneal endothelial damage remains. We have performed this procedure over 400 individuals and to date have had no cases of endophthalmitis and no retinal detachment. In addition, by following endothelial cell count we have observed no evidence of corneal endothelial damage. VEGF inhibitors can be introduced into the pseudophakic eye safely using a perilimbic approach – and potentially even with phakic eyes too. This method avoids scleral and retinal injury, reduces the risk of endophthalmitis and central retinal vein occlusion, and can be safely performed by ophthalmologists who aren’t retinal specialists.
The Perilimbic Intravitreal Injection Procedure
- After instilling a mydriatics agent (Mydriacyl 0.5%, Alcon, Dallas, TX, USA), the eyelids are scrubbed with 1% povidone iodine. A drop of povidone iodine is instilled into the eye, followed by a drop of the local anesthetic 0.5% tetracaine hydrochloride (AlconLaboratories, Dallas, TX USA). The eye is draped with Tegaderm dressing (3M, St. Paul, MN, USA), a lid speculum is placed and thepatient is placed supine under the operating microscope with light off.
- A Mastel ring light and fixation light are used to fixate the eye. Using an Alcon single use ophthalmic 15° angled knife, a 0.4 mm paracentesis is made at the limbus at 11 o’clock.
- A 30-gauge irrigating, 5 mm angled cannula, attached to a 1.0 ml syringe is fitted into the paracentesis incision and advanced through the limbus, over the iris, across the edge of the intraocular lens into the anterior vitreous in between the zonules – at this point it can be visualized within the posterior chamber.
- Next, 0.05 cc of bevacizumab is injected into the posterior chamber behind the IOL (Figure 1b), and the cannula is removed immediately so as not to chafe the iris.
- After delivery of the bevacizumab, the paracentesis site is hydrated and the fundus examined by indirect ophthalmoscopy to insure normal central artery perfusion.
Murad Sunalp is President of Sunalp Laser Vision, Tulare, CA, USA. Lindsey Buchbinder is a medical student at St. George’s University, True Blue, Grenada. Myhidin Shehu is the Medical Director of Sunalp Laser Vision.
