- Many prior radial keratotomy patients are now presenting to ophthalmologists with vision problems caused by irregular ametropia, including hyperopic shift over time
- These cases can seem daunting, but it’s possible to produce great outcomes with the right approach for vision correction
- LASIK is one possible approach – but it may cause more problems than it solves, and could further destabilize the cornea
- Laser corneoplastique is an advanced form of surface laser surgery involving manual epithelium removal, which helps the cornea heal, and decreases surface irregularities
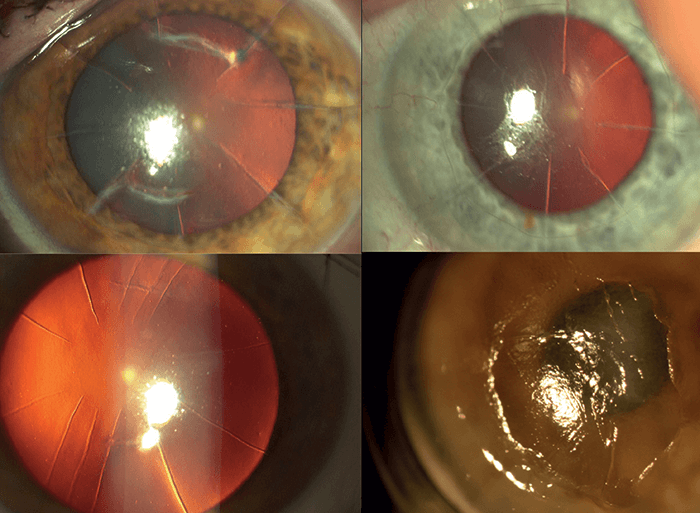
Radial keratotomy (RK) was a very popular technique in the eighties. A series of radial, deep corneal incisions (Figures 1 and 2) flattened the cornea – and corrected myopia. But although it served thousands of patients well at the time, it also resulted in hyperopic shifts over time, creating irregular corneas with long-term visual instability. Now, there are thousands of patients worldwide who underwent RK and are now presenting to their doctors with vision issues – it’s essentially a refractive epidemic. But I believe it’s possible to “turn back the clock” with the right approach.
Tackling the refractive epidemic head on
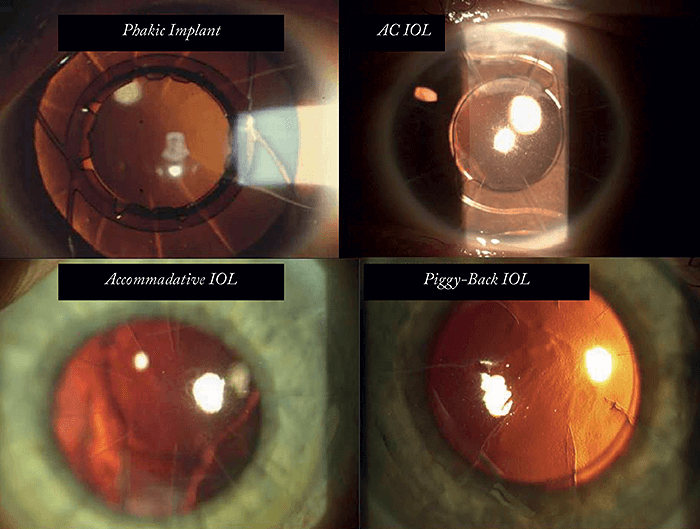
The list of potential problems when dealing with post-RK corneas can be long: the size and placement of the incisions and scarring can leave you dealing with a particularly fragile cornea. The next problem is biometry: taking accurate measurements in these eyes can be particularly challenging – and predicting outcomes is also difficult. It’s important to always begin surgery with the right mindset: don’t be intimidated by the number or pattern of RK cuts you see in your patient’s cornea (see Figure 1). Instead, go into surgery with the belief that despite the cuts, it’s possible for your patient to achieve unaided emmetropia and 20/20 vision. There is a whole spectrum of corneal and lenticular techniques that can be used to rehabilitate vision, but I shall restrict the discussion here to the use of my laser corneoplastique approach (1), which can not only correct the full range of refractive errors that can result from RK but also its associated pathologies. Let’s review the “inside-out” and “outside-in” lens implant-based combination protocols. “Outside-in” is an approach for situations when corneal topography cannot be measured; for example, in cases of corneal scarring, post-RK irregular ametropia, or post-LASIK ectasia. The cornea is first made measurable using procedures like Intacs, lamellar keratoplasty or corneal collagen crosslinking, and then cataract surgery is performed once accurate biometry and IOL calculations can be made. The “inside-out” approach is used when the cornea is measurable but still needs refractive correction – in these cases, the cataract surgery is performed first, with the aim of correcting residual refractive error afterwards using ablation.Imagine the post-RK cornea as a sheet of well-adhered but broken tiles. The returning epithelium following this laser surface ablation approach not only covers and heals the cornea but also decreases surface irregularities and instability – over and above the refractive correction achieved with the excimer laser alone. Anecdotally, I have also noted this procedure results in greater vision stability. After over two decades of correcting virtually every variety of post-RK cornea and their associated pathologies to give these patients emmetropic vision, I believe this approach produces the best possible outcomes. Another option for post-RK corneas is, of course, regular LASIK surgery – but this should be avoided. In my view, LASIK on RK corneas is not the best idea, both anatomically and physiologically: it horizontally destabilizes a structure that is already vertically compromised. Think of a cake cut into eight pieces, nicely held on a platter. Now, take a knife and cut through all eight pieces with a single horizontal swipe – you are highly likely to dislodge some pieces. By performing LASIK on these eyes, you place the patient at a high risk of tissue displacement, refractive fluctuations, corneal ectasia, irregular astigmatism, epithelial ingrowth at flap incision intersections, along with dry eye and tear film instability. Just because the approach works in some cases, doesn’t mean it’s the best approach here!
Delicate but decisive
Laser corneoplastique is performed as a no-flap, no-cut, surface ablation technique broadly similar to conceptual photorefractive keratectomy (PRK) surgery, but with advanced protocol and manual epithelium removal. The epithelium should not be removed with alcohol or toxic chemicals, but instead with a blunt, modified diamond-dusted spatula – the Gulani LASIK spatula. I have classified this process into centripetal (removal from the periphery to the center) and centrifugal (removal from the center to the periphery) techniques. I use a centripetal technique in most post-RK cases with no additional corneal issues like prior LASIK surgery, and I find that a centrifugal technique is more applicable in cases where there are other associated corneal issues, such as LASIK flaps, scars, or very unstable corneas with deep intersecting RK cuts. It’s important to bear in mind how fragile these corneas are – your movements should be gentle, but decisive and fast – this will lead to less irregularity and a lower chance of creating false planes including the opening of RK incisions. Epithelium removal is the most important physical step in these cases – it reveals the underlying cornea and the work of the previous surgeon, and no number of topographies or OCT images can give you this information. The most important step of all comes next: refraction-based laser corneoplastique. Your refraction through these corneas has to be very accurate and you must check it repeatedly during preoperative visits. Using the 193 nm argon fluoride excimer laser at 120 MJ/cm2 at a modified pulse frequency, I proceed with ablation, followed by Mitomycin C0.02% washed by BSS at completion for 20 seconds. In my experience – and in all cases – the patient will begin to see more clearly right there under your laser. Place a bandage contact lens on this cornea, and the procedure is completed.Why should you choose a surface ablation technique, such as laser corneoplastique? In essence, you’re taking away all the negatives of incisional keratorefractive surgery (including regular LASIK), so that you are sculpting with a sub-micron precision laser to get the shape you want. You’re also able to correct the entire range of refractive errors, address irregular astigmatism, and correct associated corneal scars. As I always say: refraction is a must and accuracy is absolutely paramount – in fact, it is the single most important defining factor of your success. The number of cuts, the pattern, or how “horrible” they look doesn’t matter at all. A medication protocol of antibiotic and anti-inflammatory drops for two weeks and steroid drops on a taper from 4 to 1 per day over four weeks is followed. I remove the bandage contact lens by day five, and the majority of patients had epithelial closure by this time. No patients reported any pain, even when questioned, underscoring the fact that the surgery is comfortable for patients, and provides vision recovery and results that even these highly demanding patients find satisfactory.
A winning combination
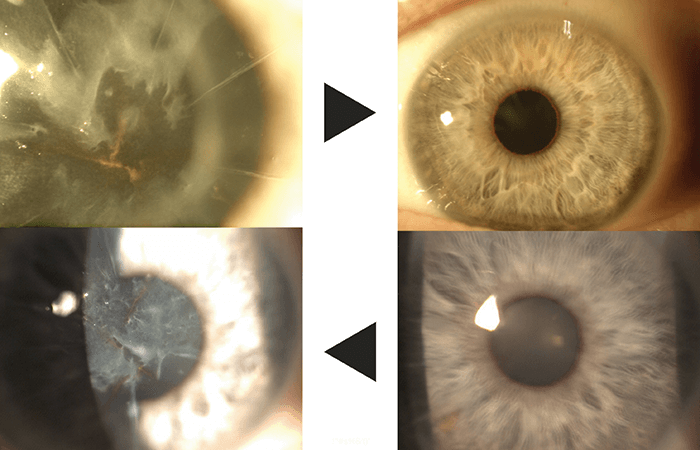
Laser corneoplastique in post-RK eyes can also be combined with cataract surgery, as many of these patients are now of the age where cataract surgery might be indicated, and clearing the cornea of scars or irregular refractive errors with this procedure, combined with cataract removal should lead to the best possible postsurgical visual outcomes (Figure 3). Excimer laser use – as an advanced version of PRK – in laser corneoplastique mode is a safe, effective and predictable technique to correct refractive errors in post-RK eyes. Instead of weakening an already weakened cornea, the returning epithelium decreases fluctuations, improves anterior corneal smoothness and shape, which, in turn, makes the RK cuts (no matter the number) less relevant visually. It’s like placing a new carpet over broken tiles...Arun Gulani is the founding Director and Chief Surgeon of the Gulani Vision Institute in Jacksonville, Florida, USA and has specialized in over 48 vision corrective techniques including advanced LASIK, premium cataract and custom corneal surgery. An award- winning inventor of numerous surgical instruments and techniques, Gulani is a widely published author and international instructor to eye surgeons worldwide. Aaishwariya Gulani, is a pre-med undergraduate at Wharton School of Business at the University Pennsylvania.
Arun Gulani is a consultant for Ocular Therapeutix, Oculus and MARCO. Aaishwariya Gulani reports no conflicts of interest.
A video of the laser corneoplastique technique is available online at: https://youtu.be/OmPtGwT4eQs.
References
- AC Gulani, “Corneoplastique™: art of vision surgery”, Indian J Ophthalmol, 62, 3–11 (2007). PMID: 24492495.
