UWF imaging and navigated peripheral optical coherence tomography (OCT) are redefining how clinicians diagnose and manage retinal diseases. By extending visibility beyond the posterior pole into the peripheral retina, these technologies enable earlier detection of subtle pathologies, more precise monitoring, and ultimately, more effective and retina-sparing interventions.
These advances took center stage during an Optos industry session at this year’s EURETINA Congress in Paris (September 4–7, 2025). An expert panel – Professor Srinivas Sadda, Dr. Jacques Bijon, Dr. Daniela Bacherini, and Professor Paulo-Eduardo Stanga – shared both clinical evidence and real-world experiences, illustrating how UWF imaging combined with navigated peripheral OCT is reshaping the standard of care across a spectrum of retinal diseases.
Monitoring GA
Starting the proceedings, Professor Sadda, Director of Artificial Intelligence & Imaging Research at the Doheny Eye Institute, and Professor of Ophthalmology at the University of California, Los Angeles (UCLA) Geffen School of Medicine, explored the evolving understanding of monitoring age-related macular degeneration (AMD).
Using UWF autofluorescence (FAF) imaging on the Optos platform, he recounted how his team identified peripheral retinal abnormalities, such as punctate hyperautofluorescence, reticular pigmentary changes, and peripheral atrophy, that correlated with advanced AMD and may be useful for predicting progression.
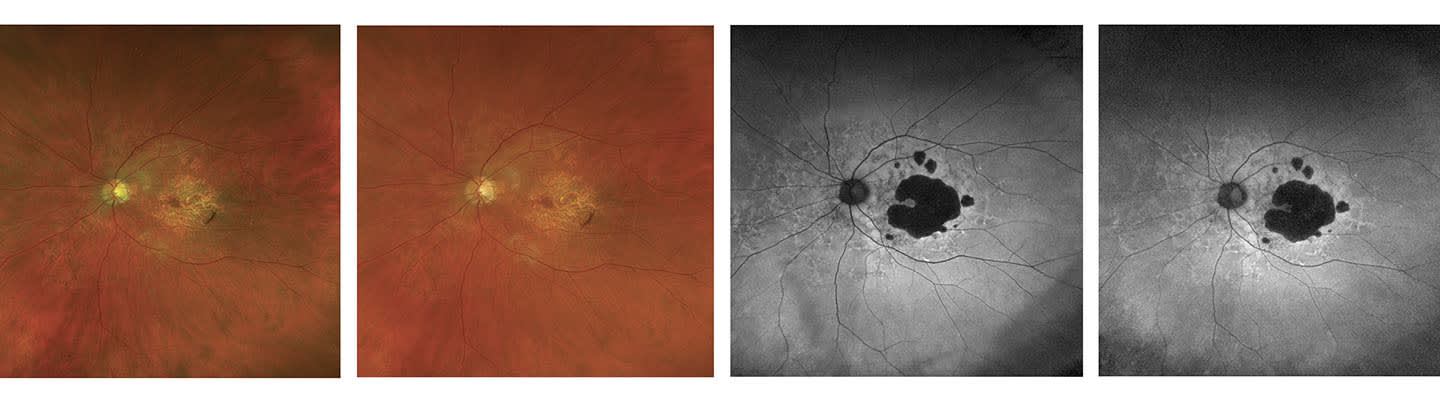
“But can we reliably use UWF FAF imaging to identify and quantitatively monitor geographic atrophy (GA)?” he asked.
While typical blue-wavelength autofluorescence is the primary outcome measure in GA trials, Prof. Sadda noted its drawbacks – patient discomfort and limited foveal assessment due to macular pigment. “That’s where green-wavelength autofluorescence has real potential value,” he said, offering better comfort and clearer foveal visualisation. In a study of 138 eyes, only using green-wavelength UWF autofluorescence, a lower rate than typically seen with blue-wavelength imaging. In those few ungradable cases, age-related choroidal atrophy (ARCA) was present, and Optos colour imaging still enabled reliable assessment.
GA lesions, then, can be reliably measured and accurately graded using UWF FAF (and colour) imaging, Sadda observed. “As the primary tools to monitor GA progression, they are especially valuable in the era of GA therapeutics.”
Optos UWF imaging, Prof. Sadda concluded, is “a critical asset in AMD care, offering both diagnostic depth and practical flexibility – especially as emerging findings suggest AMD may be a pan retinal disease.”
Managing high myopia
Dr. Jaques Bijon, a paediatric ophthalmologist at the Adolphe de Rothschild Foundation in Paris, presented insights into the role of UWF imaging in managing high myopia in children. Observing that “the prevalence of myopia is increasing dramatically worldwide,” he explained that early-onset myopia raises the risk of high myopia and, later in life, the risk of retinal detachment, monitoring the peripheral retina to detect early signs of retinal stress and degeneration is therefore crucial.
Studies from 2010 to 2024, Dr. Bijon pointed out, report that 33–61% of highly myopic children exhibit peripheral lesions (2,3). “However,” he continued, “detecting these lesions is not straightforward in children. We can’t always examine each retinal quadrant as thoroughly as we would in adults.”
Primarily using Optos, Dr. Bijon was part of a team conducting a retrospective, crosssectional study involving 160 eyes from 89 children aged 4–17. Inclusion criteria required documented peripheral retinal exams or ultra-widefield imaging. Among the study’s finding were that 54.4% of eyes had at least one peripheral lesion; lesions were more common in older children; 43% of affected eyes had multiple lesions; and of the most common lesions, 60% of patients had at least one lesion, with bilateral involvement in 64% of those cases.
Dr. Bijon explained that UWF imaging proved “an excellent tool for baseline documentation and monitoring, especially in children with limited cooperation, because it offers these really broad fundus views, even in small pupils.” Emphasising UWF imaging’s role in improving diagnosis and guiding treatment in paediatric myopia care, he concluded, “It has been very helpful in my clinic, and has really helped me anticipate and ultimately improve long-term visual outcomes.”
Diagnosing peripheral retinal degenerations
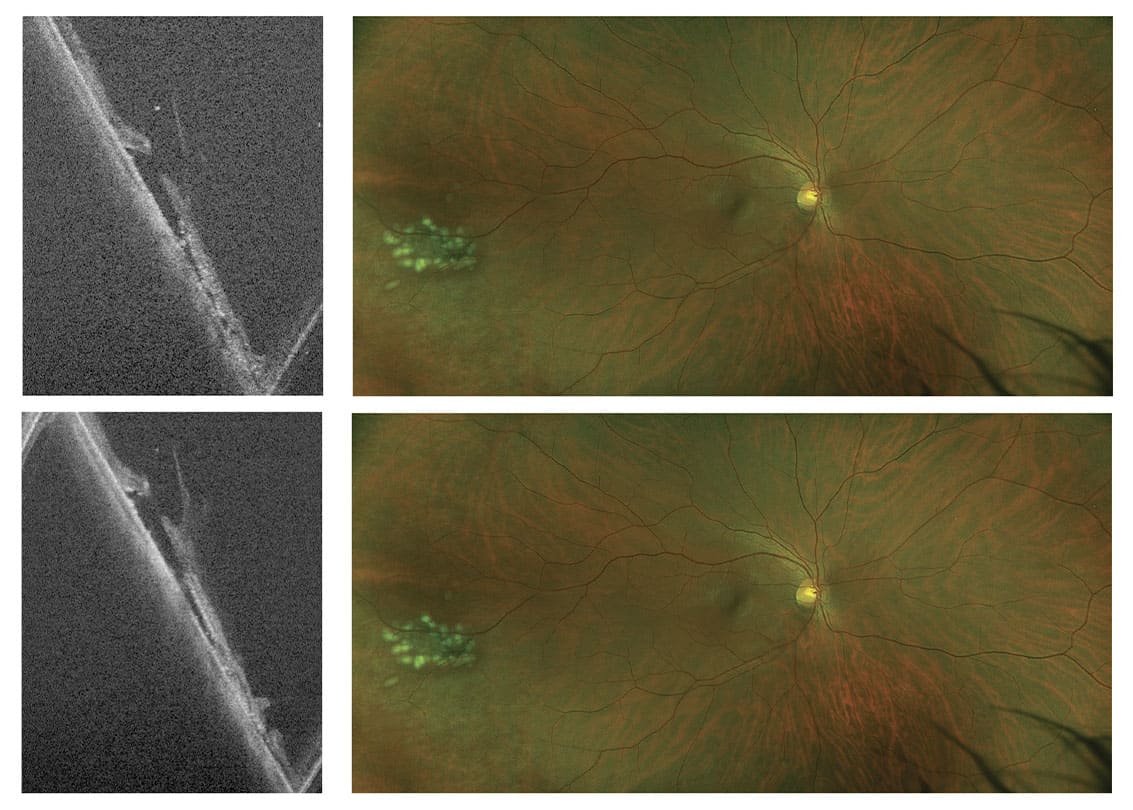
Dr. Daniela Bacherini of the University of Florence discussed the transformative role of ultra-widefield imaging and peripheral OCT in diagnosing peripheral retinal degenerations. Hitherto overlooked, the field is “entering a new era, thanks to UWF imaging,” she said. So,” she asked, “can we rely on UWF imaging to better stratify risk of retinal detachment, particularly peripheral OCT?”
“As we know, the macula has traditionally been the primary focus of OCT imaging,” Dr. Bacherini explained. But OCT has now moved to the periphery with WF and UWF imaging techniques, with advanced features like swept-source OCT that can capture up to 200° of the retina in detail.
Dr. Bacherini’s study aimed to characterise different types of peripheral retinal degeneration, using UWF sweptsource navigated OCT, integrated with the scanning laser ophthalmoscope on Optos’ Silverstone platform. The study revealed that peripheral OCT findings altered clinical decisions in 44% of cases, she noted, often prompting laser treatment over observation. UWF guided OCT enabled detection of subtle features such as vitreoretinal traction, subretinal fluid, and retinal holes that were not visible via ophthalmoscopy. Even if it can’t replace fundus examination, it can help differentiate lesion types and potentially assess risk for retinal detachment.
Dr. Bacherini emphasised the tool’s value in improving diagnosis, guiding treatment, enhancing patient education, and supporting telemedicine. She concluded that peripheral OCT offers meaningful insight into peripheral retinal diseases and may help standardise intervention criteria in the future.
The transformative role of UWF Imaging
Professor Paulo-Eduardo Stanga delivered an insightful presentation on the clinical impact of Optos Silverstone and the evolution of UWF imaging in retinal care. He underscored that traditional ophthalmoscopy and conventional imaging methods often fail to capture the peripheral retina, where many pathologies begin. He argued that UWF technology has fundamentally reshaped modern ophthalmology. “It was really Optos that changed the landscape and allowed the democratisation of UWF in 2010,” he noted, referring to how Optos made ultrawidefield imaging broadly accessible to clinicians, moving it from a specialised tool used in select centers to a standard part of everyday retinal practice.
Silverstone’s integration of UWF imaging with navigated peripheral OCT provides clinicians with unparalleled ability to detect, document, and monitor subtle lesions. By correlating OCT cross-sections with UWF modalities including angiography, physicians can diagnose earlier and treat more precisely, minimizing unnecessary retinal damage. Stanga illustrated cases ranging from diabetic retinopathy to lattice degeneration, retinal holes, and subclinical detachments – conditions where early detection in the periphery can make a decisive difference. “With Optos it is very easy because you know exactly where the scan is being done,” he explained, emphasizing how the system improves accuracy and efficiency.
The technology, he argued, does not just enhance diagnostic precision but also changes clinical decision-making. Real-time navigation and documentation empower more confident, data-driven treatment strategies, especially in complex cases such as proliferative diabetic retinopathy or high-risk retinal tears.
Stanga concluded with a clear endorsement: “I can’t imagine being without this technology in my clinic.” For him, Optos Silverstone has become indispensable – both a diagnostic cornerstone and a catalyst for more retina-sparing, patient-centered care.
The discussions at EURETINA 2025 underscored a clear consensus UWF imaging, particularly when combined with navigated peripheral OCT, is no longer a luxury but an essential component of modern retinal care. From monitoring GA progression and managing pediatric high myopia to diagnosing peripheral degenerations and guiding advanced vitreoretinal treatments, Optos technology is driving earlier, more confident, and more precise decision-making.
References
- R. Abbasgholizadeh et al., “Comparison of Blue-Light Autofluorescence and Ultrawidefield Green-Light Autofluorescence for Assessing Geographic Atrophy,” Ophthalmol Retina, 8, 987 (2024).
- AS Bansal, GB Hubbard 3rd, “Peripheral retinal findings in highly myopic children < or =10 years of age,” Retina, 30 (4 Suppl), 15 (2010).
- Y Du et al., “Complications of high myopia: An update from clinical manifestations to underlying mechanisms,” Adv Ophthalmol Pract Res., 4, 156 (2024).
- J Zeilinger et al., “Comparing an Advanced Monofocal With a Non-diffractive Extended Depth of Focus Intraocular Lens Using a Mini-Monovision Approach,” American Journal of Ophthalmology, 271, 86 (2025).
- KM Rocha, “Expanding depth of focus by modifying higher-order aberrations induced by an adaptive optics visual simulator,” J Cataract Refract Surg., 11, 1885 (2009).
- R Schmid et al., “Depth of focus of four novel extended range of vision intraocular lenses,” Eur J Ophthalmol., 1, 257-261 (2023).
- G Barret et al., “Extending Range of Vision with Advanced Technology IOLs,” mivision, April 1, 2024.
