
Historically, endophthalmitis was believed to represent a failure of surgical technique. For example, in the 1971 Doyne Memorial Lecture, Leopold wrote, “There must be both a loophole in technique and an opportunistic organism with the necessary characteristics to penetrate the loophole” (3). More recently, the consensus is that the rate of endophthalmitis cannot be reduced to zero – in other words, “endophthalmitis is not a ‘never event’” (4).
Prior rates of postoperative endophthalmitis were lower than one might think. Lister’s initial publication on antisepsis for general and orthopedic surgery was published in 1867 (5), leading to the gradual introduction of the process into eye surgery in the 1870s. In 1874, Horner reported that his “failure rate” of cataract surgery declined from 6.6% from 1867-1870 (prior to antisepsis) to 1.5% from 1870-1875 (with antisepsis) (6). Similarly, Leopold reported a reduction of endophthalmitis rates following cataract surgery from about 2% in 1920 to about 1% in 1940, which he attributed to further improvements in aseptic technique.(3) Allen and Mangiaracine reported further reductions in endophthalmitis rates from 1.16% from 1945-1950 to 0.11% by 1964, which they attributed to the routine use of prophylactic topical and subconjunctival antibiotics (7).
This very impressive drop in endophthalmitis rates was followed by diminishing further improvements. Current reported rates of endophthalmitis following cataract surgery vary widely, but generally range from about 0.02% to 0.2%. This seems surprising when one considers the many advances in cataract surgery over the past 60 years, including phacoemulsification, smaller incisions, and foldable intraocular lenses (IOLs).
In an effort to further reduce rates of endophthalmitis, many investigators have studied the use of routine prophylactic intracameral antibiotics. This practice is currently considered standard therapy in most of Europe and in many parts of the US. The strongest evidence in favor of prophylactic intracameral antibiotics comes from a randomized clinical trial (RCT) published by the European Society of Cataract & Refractive Surgeons (ESCRS) in 2007, which reported that the use of intracameral cefuroxime was associated with approximately a 5-fold reduction in the rates of endophthalmitis, from about 0.35% to about 0.07% (8). However, these results have been criticized due to the high rates of endophthalmitis without intracameral cefuroxime (0.35%), which exceeds the rate reported by Allen and Mangiaracine in 1964 (0.11%) and may have biased the results in favor of cefuroxime.
Treatment of endophthalmitis
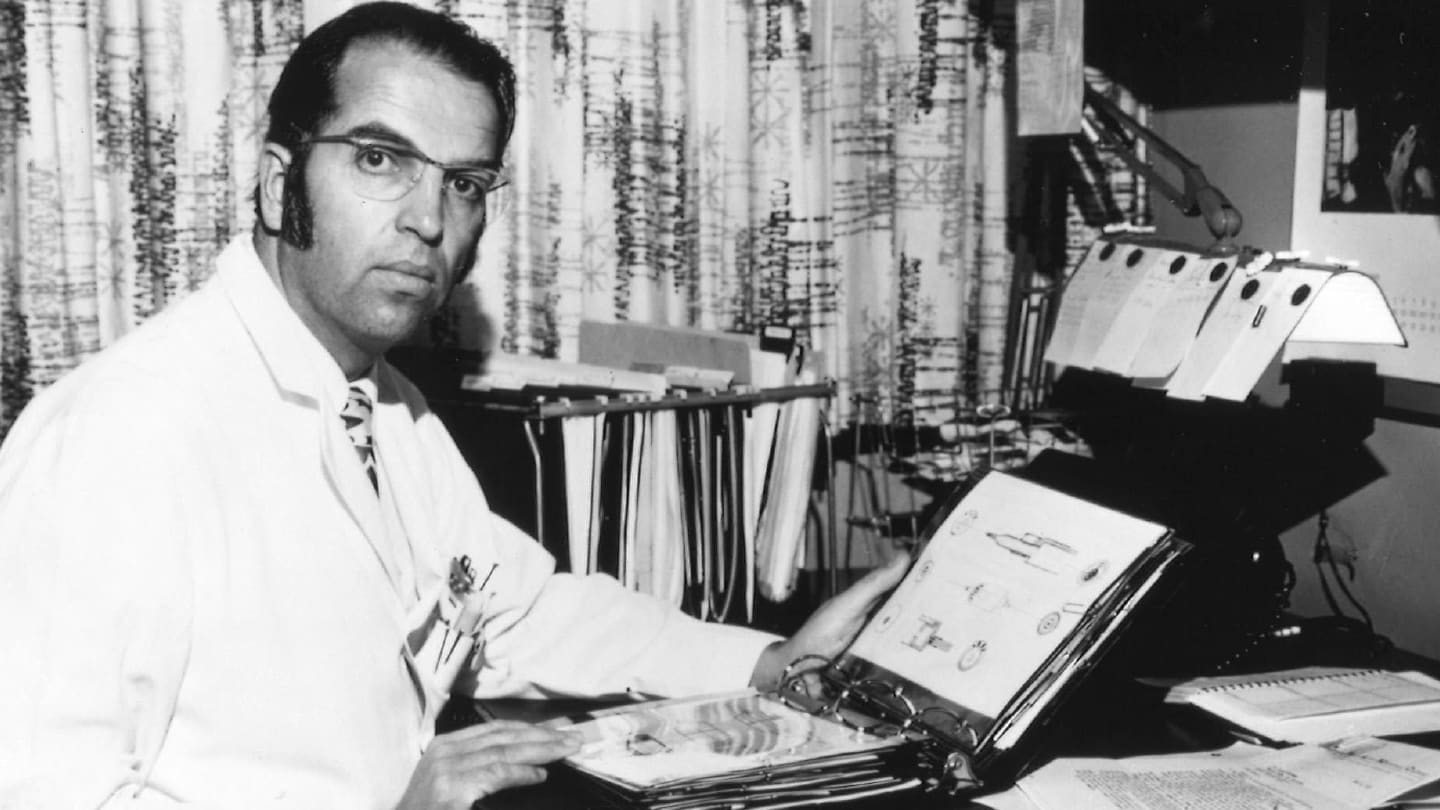
Before the introduction of antibiotics, treatments for postoperative endophthalmitis included antiserum, mercury oxycyanide, topical mercurochrome, intravenous typhoid vaccine, intramuscular injection of boiled milk, and local x-rays (1,2). After the introduction of antibiotics in the early 1940s and until the early 1970s, standard treatment for endophthalmitis was hospitalization and intravenous antibiotics, with or without adjunctive topical, subconjunctival, and sometimes intracameral antibiotics. Unfortunately, treatment outcomes were generally poor. For example, Forster (Figure 1) wrote in 1974 that “infected eyes are usually lost” (9).

The generally unsatisfactory outcomes observed using systemic and subconjunctival antibiotics led to the investigation of intravitreal delivery. Intravitreal antibiotics were reported in a rabbit model of endophthalmitis by Peyman and colleagues using methicillin (10) and amphotericin B (11) in 1973. The following year, successful treatment of patients with postoperative endophthalmitis with intravitreal antimicrobials was reported by Peyman and Herbst (12). In this same year, Forster also reported generally successful treatment of 33 patients with endophthalmitis due to various etiologies, including following cataract surgery (9).
The development of pars plana vitrectomy (PPV) is generally credited to Machemer (Figure 2) and colleagues in 1971 (13), although similar techniques were also reported by Peyman and colleagues at approximately the same time (14). PPV was proposed to offer many benefits, including debulking infected vitreous, obtaining larger samples for culture, and allowing better diffusion of antibiotics in the vitrectomized eye.
The Endophthalmitis Vitrectomy Study (EVS), an RCT, was conducted from 1990-1994 by Doft (Figure 3) and coinvestigators through the National Eye Institute. The results, published in 1995 (16), compared PPV with vitreous tap and injection (TAP) with intravitreal vancomycin and amikcacin, as well as intravenous amikacin and ceftazidime (or oral ciprofloxacin for penicillin-allergic patients) versus no systemic antibiotics. The major findings of the EVS were:
In patients presenting with visual acuity (VA) of hand motions or better, there was no significant difference in visual outcomes between PPV and TAP
In patients presenting with VA of light perception, visual outcomes were significantly more favorable with PPV
Intravenous amikacin and ceftazidime (or oral ciprofloxacin for penicillin-allergic patients) did not significantly affect visual outcomes

Perhaps surprisingly for a 30-year old study, the findings of the EVS are generally followed to this day. The major exception is that most physicians substitute ceftazidime or another third-generation cephalosporin for amikacin, which is associated with macular toxicity. Another exception is the use of systemic antibiotics, especially later-generation fluoroquinolones, which are commonly used in Europe and other parts of the world, but less often in the US (17). Moreover, early vitrectomy is used more often in Europe than in US (18).
References
- LJ Rohowetz et al., “Endophthalmitis Then and Now,” Retinal Physician, 22, 8 (2025). https://retinalphysician.com/issues/2025/may/endophthalmitis-then-and-now/
- SG Schwartz et al., “Postoperative endophthalmitis: the history of its prophylaxis and treatment,” in Hirschberg History of Ophthalmology: The Monographs, Vol. 17: A New History of Cataract Surgery, Part 2: From 1751 Through the Modern Era, CT Leffler (ed.), Wayenbourgh (Kugler), Amsterdam (2024).
- IH Leopold, “Management of intra-ocular infection,” Trans Ophthalmol Soc UK, 91, 577 (1971).
- AP Schachat et al., “Endophthalmitis is not a ‘never event’,” Ophthalmology, 119, 1507 (2012).
- J Lister, “On the antiseptic principle in the practice of surgery,” Br Med J, 2(351), 246 (1867).
- CT Leffler, S Bansal, “Angle-closure glaucoma since 1871,” in The History of Glaucoma, Hirschberg History of Ophthalmology The Monographs Volume 15, CT Leffler (ed.), Wayenborgh Publications, Amsterdam (2020).
- HF Allen, AB Mangiaracine, “Bacterial endophthalmitis after cataract extraction: a study of 22 infections in 20,000 operations,” Arch Ophthalmol, 72, 454 (1964).
- Endophthalmitis Study Group. European Society of Cataract & Refractive Surgeons, “Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors,” J Cataract Refract Surg, 33, 978 (2007).
- RK Forster, “Endophthalmitis: diagnostic cultures and visual results,” Arch Ophthalmol, 92, 387 (1974).
- MJ Daily et al., “Intravitreal injection of methicillin for treatment of endophthalmitis,” Am J Ophthalmol, 76, 343 (1973).
- AJ Axelrod, GA Peyman, “Intravitreal amphotericin B treatment of experimental fungal endophthalmitis,” Am J Ophthalmol, 76, 584 (1973).
- GA Peyman, R Herbst, “Bacterial endophthalmitis: treatment with intraocular injection of gentamicin and dexamethasone,” Arch Ophthalmol, 91, 416 (1974).
- R Machemer et al., “Vitrectomy: a pars plana approach,” Trans Am Acad Ophthalmol Otolaryngol, 75, 813 (1971).
- GA Peyman, NA Dodich, “Experimental vitrectomy: instrumentation and surgical technique,” Arch Ophthalmol, 86, 548 (1971).
- PR Pavan, JH Brinser, “Exogenous bacterial endophthalmitis treated without systemic antibiotics,” Am J Ophthalmol, 104, 121 (1987).
- Endophthalmitis Vitrectomy Study Group, “Results of the Endophthalmitis Vitrectomy Study: a randomized trial of immediate vitrectomy and of intravitreous antibiotics for the treatment of postoperative bacterial endophthalmitis,” Arch Ophthalmol, 113, 1479 (1995).
- A Grzybowski et al., “The role of systemic antibiotics in the treatment of endophthalmitis: a review and an international perspective,” Ophthalmol Ther, 9, 485 (2020).
- DC Sousa et al., “Pars plana vitrectomy in acute endophthalmitis: The Manchester Series,” Ophthalmic Surg Lasers Imaging Retina, 53, 96 (2022).
