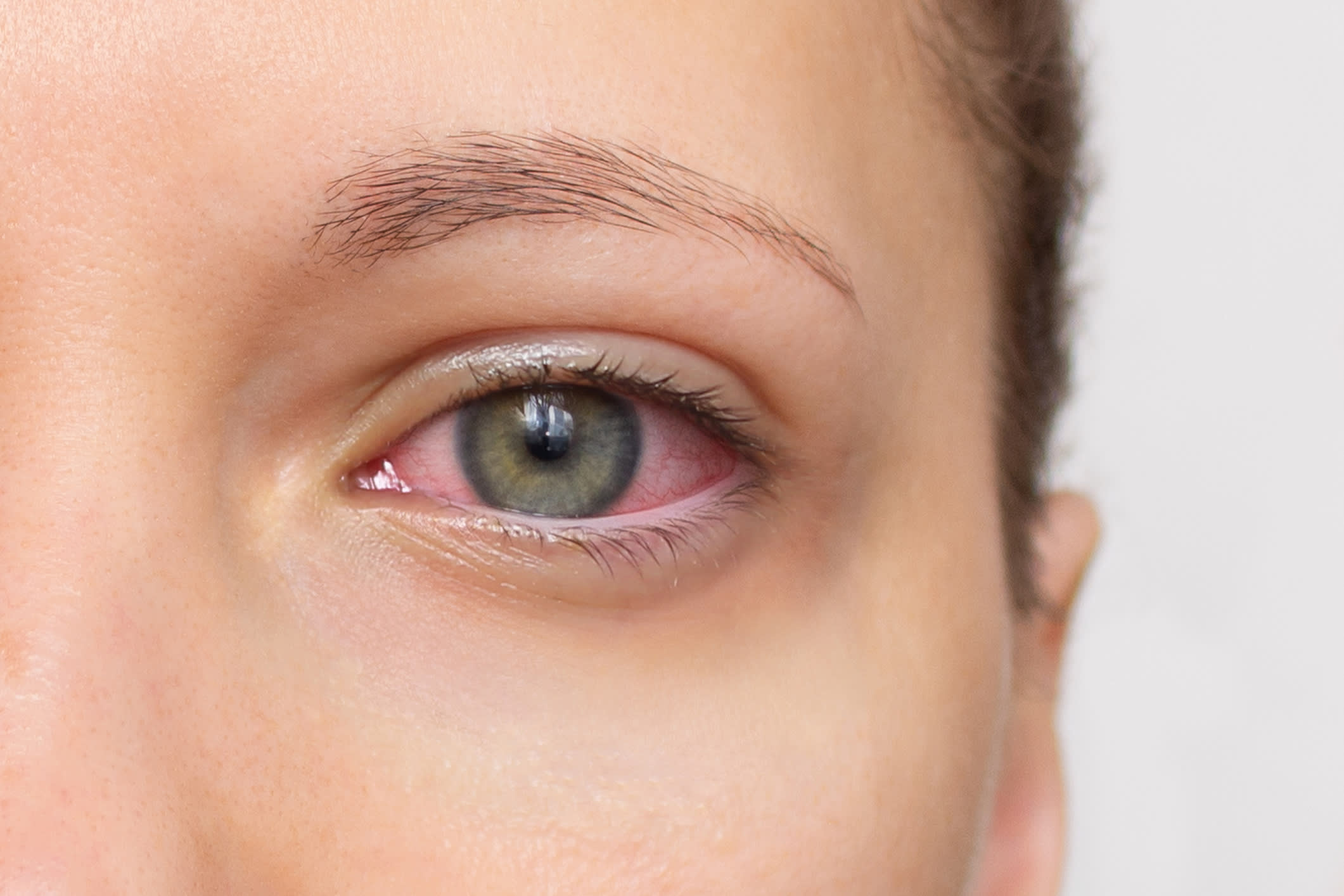
Uveitis remains a leading cause of preventable blindness worldwide. Now, evidence from a recent JAMA review is prompting clinicians to reconsider how they approach diagnosis and management.
The newly gathered data show how geography and patient demographics can significantly shape both presentation and underlying cause of uveitis. In high-income countries like the UK, infectious triggers such as toxoplasmosis and herpes account for a relatively small proportion of cases. However, in many lower- and middle-income regions, infections – including tuberculosis and HIV-related uveitis – are much more common. With increasingly diverse patient populations, clinicians need to remain alert to these variations, and travel and social history can often provide vital diagnostic clues that laboratory tests might miss.
Uveitis tends to affect younger adults, with most cases presenting between ages 20 and 50. Gender patterns can also offer helpful insights: HLA-B27-associated uveitis is more common in men, while conditions like multiple sclerosis-related and juvenile idiopathic arthritis-associated uveitis more often affect women. Recognising these demographic signals can sharpen differential diagnosis, especially when systemic features are present.
Perhaps the most striking change in recent years has been the evolution of treatment. The reliance on corticosteroids alone is giving way to targeted therapies grounded in robust clinical evidence. While anterior uveitis often still responds well to topical steroids, more complex forms – particularly intermediate and posterior uveitis – frequently require systemic immunosuppression. Agents like methotrexate and mycophenolate are increasingly used as first-line therapies.
For patients with refractory disease, biologic agents such as adalimumab have dramatically improved outcomes. The VISUAL trials demonstrated that adalimumab not only extends the time to treatment failure but also offers many patients the possibility of long-term remission – something that was much harder to achieve just a decade ago.
Early recognition and prompt treatment remain critical. Ongoing inflammation can lead to permanent complications such as cataracts, glaucoma, and macular oedema. Even with effective therapy, these complications remain common, underscoring the need for early referral to ophthalmology when uveitis is suspected. Same-day referral is essential if patients present with significant vision loss, visual distortion, or severe pain.
As newer therapies continue to emerge, clinicians are better equipped than ever to prevent vision loss and offer patients meaningful long-term control. Staying vigilant to global patterns, demographic clues, and the expanding therapeutic landscape will be key to improving outcomes in uveitis care.
