
Dr. I. Paul Singh
The Ahmed ClearPath® is a novel valveless glaucoma drainage device (GDD) approved in 2019 by the US Food and Drug Administration for the management of glaucoma. Dr. I. Paul Singh, glaucoma specialist and President of The Eye Centers of Racine & Kenosha, Wisconsin, USA, and early adopter of the Ahmed ClearPath, shares his perspective on the benefits of the device for both the surgeon and patient.
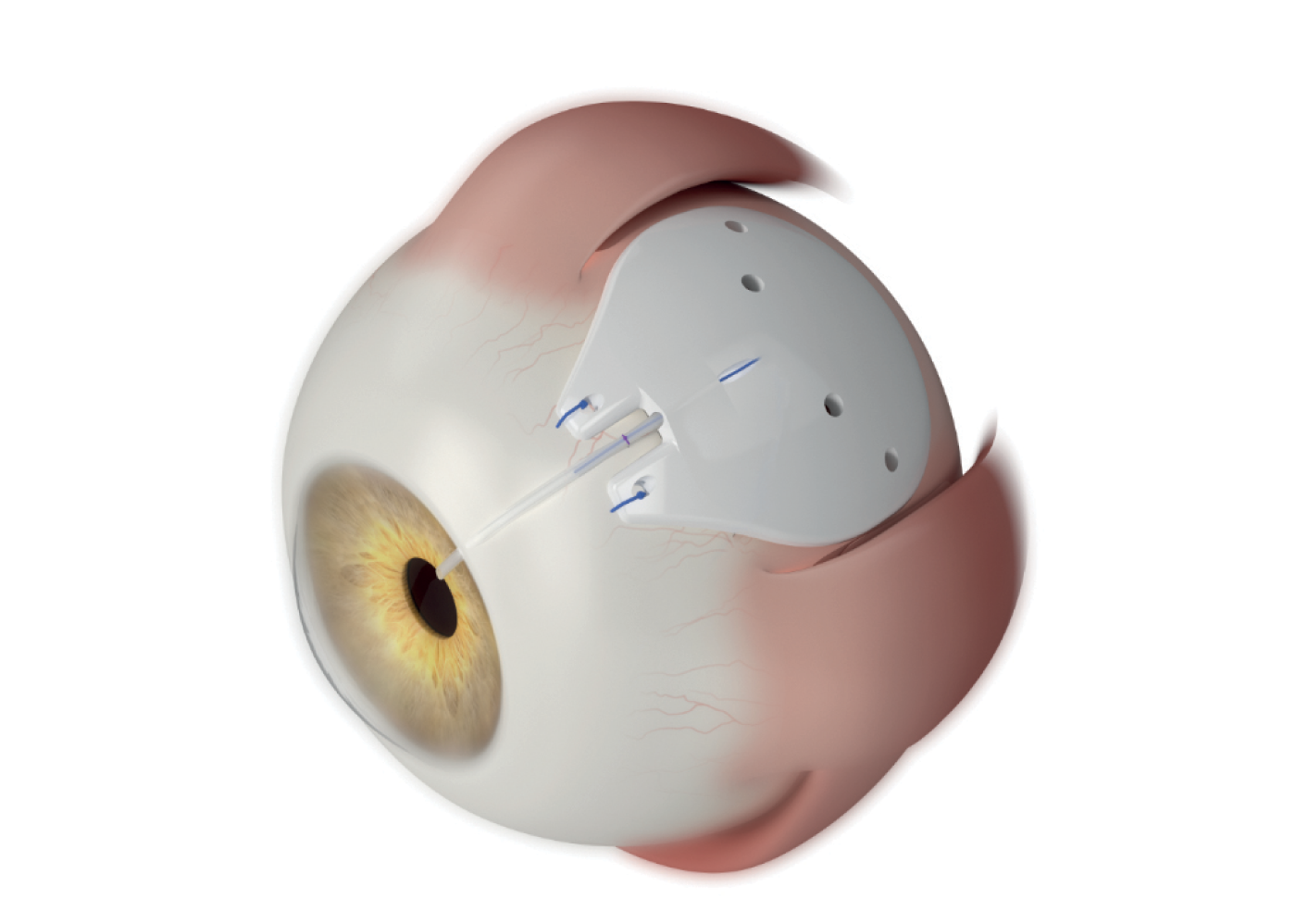
Of the many unique features to the Ahmed ClearPath is the importance of the device’s low profile, Singh says; “the contour makes it more likely to hug the sclera, which delays the aqueous from contacting the subconjuctival space and allows for the formation of more posterior and low-lying blebs.” He adds, “I also enjoy not having to worry about identifying and manipulating the muscles with the Ahmed ClearPath 250 model, as I do with a Baerveldt. In general, not having to use a muscle hook, or place the plate under the muscles, means less dissection is needed, and thus less potential for strabismus. I feel that the ClearPath 250’s true single-quadrant design helps me perform a more efficient, cleaner surgery.”
“Taco” technique
Available in two sizes – 250 mm2 and 350 mm2 – the smaller model allows for placement between recti muscles without the need for muscle isolation, while the winged design and more posterior position of the plate on the 350 mm2 model avoid rectus muscle insertion points for those surgeons who prefer a larger plate. Singh uses the 250 mm2 “the majority of the time.” He explains, “I love the single quadrant design; it lends itself to the ‘taco technique’ nicely. In my experience, and in some data sets, the size of the plate does not necessarily impact efficacy, and yet it makes the surgical procedure more streamlined. So, for me the 250 has been my ‘go-to,’ with fantastic safety and efficacy.”
The small incision “taco” technique, a term coined by Singh himself, involves folding the Ahmed ClearPath 250 plate “into a cigar roll or a taco.” He explains, “You can use a 3-4 mm conjunctival incision around 4 mm behind the limbus, create a pocket under tenons, and then let the plate unfold like a taco or an IOL; that way your wound can remain much smaller compared to other plates that require a larger wound due to the stiffness of those plates. This can be achieved because of the ClearPath’s malleable material, “which is probably its most unique feature,” says Singh. “This is a great benefit because it means I don’t have to worry about getting under the muscles and I don’t have to use large incisions.” With a small incision size, we often see less fibrosis, and more healthy tissue, adds Singh. “This means improved healing, fewer sutures, and of course you're keeping more conjunctiva untouched, which is always a good thing.”
Anteriorly placed suture points
Another major benefit of the Ahmed ClearPath, says Singh, is that the fixation eyelets are placed more anteriorly so they are easier to access. “One of the biggest frustrations when you do tube surgery in general is trying to dissect and then suture the plate to the sclera. When the eyelets are far back, aggressive dissection is important to obtain proper exposure, which can be challenging when fighting with the tenons and conjunctiva,” Singh explains. With the Ahmed ClearPath’s anteriorly placed suture holes and enhanced curvature, “it’s more convenient to secure the plate to the sclera, which is much more efficient from a surgical technique perspective.”

Patient selection
These benefits in turn lead to more opportunity for patient selection, adds Singh. “In general, compared to trabeculectomy, I find tubes tend to have more predictable recovery and less chance for bleb leaks. This allows me to feel more comfortable offering tubes to a wider patient population.” With patients that have unhealthy conjunctiva – for example, those who have been on drops for many years and the conjunctiva has become fibrotic – Singh is “much more concerned about doing a trabeculectomy. “Instead, I’ll offer an Ahmed ClearPath earlier than a trabeculectomy,” he says. “Similarly, if I’m worried about people who are contact lens wearers, or younger patients who want to play sports, I’m much more likely to want to do a tube than do a trabeculectomy, because I know that with trabeculectomy there is a higher risk of bleb leaks, fibrosis, etc.”
Patient journey
In terms of the patients’ post-op journey, Singh keeps patients on drops after surgery “to help keep the pressure down until the tube opens up…The key is aqueous suppressants to try and keep the pressure controlled for the first month and a half, until the tube opens. The lower the IOP when the plate opens up, the less chance you have of choroidals or hypotony.”
“I think glaucoma tube surgery is something that we will always need,” concludes Singh. “I’m a big fan of MIGS, lasers, drug delivery, subconjunctival MIBS, but there are a number of patients who still need tube surgery. For me, the Ahmed ClearPath is a much needed device that has allowed me to feel even more comfortable offering tubes now than ever before.”
References
- S Dorairaj et al., “24-Month Outcomes of Ahmed ClearPath® Glaucoma Drainage Device for Refractory Glaucoma,” Clin Ophthalmol.,16, 2255 (2022). PMID: 35859670.
