Despite many years of advances in glaucoma surgery, pressure control remains a (if not the) key challenge in the management of this sight-threatening disease. Valveless shunts, such as those from Baerveldt or Molteno, require flow-restricting elements to avoid early post-op hypotony. These elements require surgical re-intervention for their removal, increasing the cost and risk of procedures. Alternatively, shunts with valve elements like the Ahmed are only able to partially avoid hypotony – and valve resistance can often lead to higher intraocular pressure (IOP) values. Ultimately, the result is more medication, and higher rates of late post-op failures.
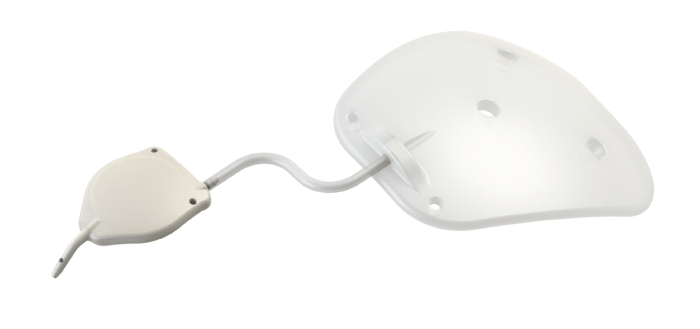
But emerging from the crowd of shunt devices is the eyeWatch system from Rheon Medical. As the world’s first – and only – adjustable glaucoma shunt, the eyeWatch is designed to drain aqueous humor in patients suffering from glaucoma, while allowing physicians to non-invasively adjust IOP. The system (see top figure) comprises the eyeWatch implant, which acts as the adjustable faucet, connected to the eyePlate – a nonvalved plate with a drainage area of either 200 mm2 or 300 mm2.
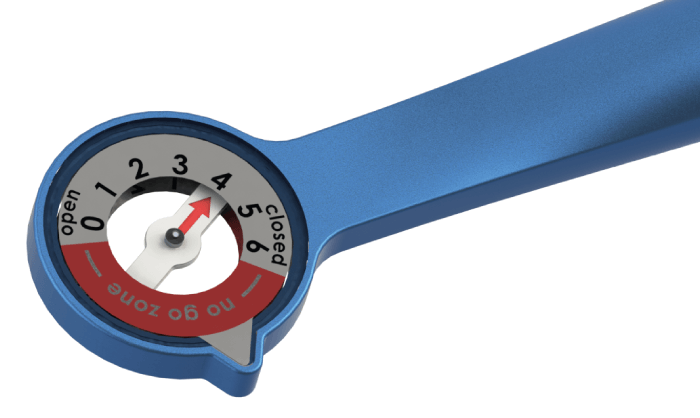
The eyeWatch mechanism allows for selective compression of an internal deformable tube, which alters its fluidic resistance, in turn adjusting the level of intraocular pressure. The IOP adjustment is performed noninvasively with the help of the eyeWatch Pen (see figure). The Pen has a magnet on one end, which – when in close proximity to the implant’s magnet – allows for the selective compression or decompression of the tube. On the other end of the eyeWatch Pen is a compass, which allows the relative position of the implant to be measured. Flow resistance can vary from a fully open position (zero resistance) to a fully closed position (high resistance). In the early post-op period, the valve can be fully or partially closed to avoid hypotony and to set the IOP levels at the optimal level for each patient. In the late post-op period, and after the bleb is fully formed, the eyeWatch can be fully opened, adding absolutely no resistance to flow, and thus keeping IOP and medication levels low.

So far, the device has seen outstanding results in more than 150 patients across six European centers. André Mermoud, a worldacclaimed surgeon in glaucoma from the Swiss Vision Network in Lausanne, Switzerland, contributed valuable clinical insights to the development of the technology. He has used the device for the past four and a half years and is enthusiastic about the results: “The eyeWatch acts on IOP from day one, avoiding hypotony and pressure spikes. I have even been able to save desperate cases of persistent hypotony after standard tube surgeries by implanting the eyeWatch. The results are truly outstanding – so much so that I have used the eyeWatch in some patients as primary surgery.”

Leon Au, a consultant ophthalmologist at the Manchester Royal Eye Hospital, UK, specializing in glaucoma, cataract and cornea, appears to echo this enthusiasm, having used the eyeWatch device in over 20 patients in the UK already. “The unique advantage of the device is the adjustability,” he says. “Every eye produces varying amounts of fluid, meaning the samesetting could produce very different results in different patients. In the past, we’ve had to adjust pressure by performing various re-interventions, such as suture lysis or stent removal, which can be unpredictable. With the eyeWatch I am able to easily and non-invasively adjust the IOP according to each patient’s needs, without the need to take them back to the operating theater. Finally, I am having an effective glaucoma drainage shunt without the associated risk attached.
The ability to titrate flow at any time during the postop period is vitally important in specific cases of persistent hypotony or in uveitic eyes – allowing the physician to maintain a certain flow resistance or continually adjust IOP."
With the eyeWatch, Au has seen clear avoidance of hypotony and related complications (0 percent persistent hypotony in all patients) and more than 90 percent of patients have been within the target IOP range (6mmHg to 18 mmHg) at one-, two- and three-year follow-up.
Further to its unique flow titration possibilities, the eyeWatch implant also avoids damage to the cornea. Though current tubes enter the anterior chamber with a comparatively
large and flexible silicone tube – often touching the cornea and causing significant endothelial damage – the eyeWatch nozzle is small and rigid, meaning it avoids the cornea and causes minimal damage. Data from clinical trials show a 5 percent endothelial cell loss at one-year follow-up, which represents a more than 50 percent decrease compared with currently marketed devices.
Clinical data also show a substantial reduction (40 percent) in cornea touch-related complications and a 90 percent reduction in corneal edema. As well as the smaller diameter of the eyeWatch tube, another significant advantage for Au is the fact that it doesn’t move once implanted. “A conventional tube is actually somewhat mobile, meaning every time a patient blinks or moves their eye, some of the tube can go in and out of it. This can lead to a significant amount of discomfort for the patient and causes corneal damage.” The eyeWatch, on the other hand, is attached to the sclera, and is therefore fixed in place. Further contributing to patient comfort is the eyePlate – which is closer in consistency to the sclera than conventional implants, making it more compatible and reducing the amount of scarring. The flexibility of the plate also makes it easier to implant.
But the eyeWatch system isn’t just useful for primary surgical interventions. “If you’ve got a patient who has already had a tube implanted but is exhibiting hypotony, then you can retrospectively fit an eyeWatch to rescue that tube,” says Au. “I think this ‘eyeWatch rescue’ procedure is quite clever as it means the device is not just useful when you come to choose the tube, but also when you’ve got an existing tube in the patient’s eye that’s giving you problems with low pressure.”
For now, Au believes physicians will each use the device in different ways: “We will obviously continue to collect data on the eyeWatch and discover if there is an optimal method for using the device, but for now the results are very exciting for the eyeWatch system.”
