
Do we always appreciate the full impact of dry eye – in all of our patients? Or are we only “scratching the surface” when it comes to managing this pernicious disease? To find out, we convened a panel of experts at the Ocular Surface Disease Forum (October 5, 2018, London; hosted by The Ophthalmologist, and sponsored by Allergan), namely:
- Sheraz Daya, Medical Director of Centre for Sight, East Grinstead, UK
- Ingeborg Stalmans, Head of the Glaucoma Clinic, University Hospitals UZ Leuven, Belgium
- Maurizio Rolando, Professor of Ophthalmology, University of Genoa, Italy
- Dawn Sim, Consultant Ophthalmic Surgeon, Moorfields Eye Hospital NHS Foundation Trust, London, UK
Sheraz Daya, Medical Director of Centre for Sight, East Grinstead, UK
Ingeborg Stalmans, Head of the Glaucoma Clinic, University Hospitals, Leuven, Belgium

Dawn Sim, Consultant Ophthalmic Surgeon, Moorfields Eye Hospital NHS Foundation Trust, London, UK

Maurizio Rolando, Professor of Ophthalmology, University of Genoa, Italy

It’s easy for us to get wrapped up in our specialties – that’s how we’ve been trained. If we are to do the best for our patients, however, we sometimes need to think (and act) outside those boxes. Consider ocular surface disease (OSD): this condition is not only troublesome in its own right, but also has a major impact on outcomes in LASIK, glaucoma and retinal surgery. Conversely, interventions associated with these and other specialties may actually trigger serious OSD – sometimes with unfortunate consequences for the doctor-patient relationship (1).
This situation suggests that we should pay more attention to proactive management of the eye’s exterior, both before and after treatment of the patient’s primary condition. Indeed, some experts assert that maintenance of a healthy ocular surface – particularly in the high proportion of ophthalmology patients who are predisposed to ocular surface problems – is key to surgical success. Unfortunately, the optimum methods of avoiding, identifying and managing OSD are not always obvious or broadly appreciated. Hence this supplement: we hope that the advice and tips outlined herein will support those ophthalmologists keen to optimise post-surgical results, and patient satisfaction, regardless of specialty.
“Conjunctival examination is critical for detection of very early dry eyes.” – Maurizio Rolando
“Use fluorescein unless there’s an indication to use lissamine green or rose bengal; for example, in Sjögren’s disease.” – Sheraz Daya
“Lissamine green is good for conjunctival staining, but fluorescein is very quick and is all you need in most cases. With fluorescein, use a yellow filter to increase contrast and reveal conjunctival fluorescein staining, which is a very good indicator of dry eye. If fluorescein is retained in the meniscus after about six minutes post-application, it demonstrates tear production is low, indicating a high-risk patient.” – Maurizio Rolando
Today’s definition of ocular surface disease (OSD) recognizes that it is a multifactorial condition (1) characterized by symptoms including tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities (2). For reasons which remain unclear, OSD is increasing in prevalence. Dietary and environmental factors may play a part – but what about iatrogenesis? It seems that a substantial proportion of patients without overt disease are significantly predisposed to OSD: in these patients, ocular interventions may trigger full-blown OSD – and the finger of blame can point squarely at the ophthalmologist.
Growing incidence – environmental factors
“My experience – 30 years in the field of ocular surface disease – indicates that the problem is significant and growing.” – Maurizio Rolando
“We live in a highly oxidative, pro-inflammatory environment: lipids quickly become oxidized, resulting in slower spreading and less effective hindering of evaporation from the tear-film. Lipid peroxidation is a chronic part of industrial life.” – Maurizio Rolando
Growing incidence – iatrogenic factors
“Eye-drop toxicity is partly due to preservatives. Glaucoma patients need chronic long-term treatment, and the toxic effect of preservatives is cumulative.” – Ingeborg Stalmans
“Intravitreal injections cause ocular surface dysfunction, not least because of the associated eye drops: anaesthetic and povidone iodine.” – Dawn Sim
Diagram rendered by the publisher.
How best to identify patients at particular risk of being tipped into serious OSD? Diligent application of a few simple diagnostic procedures – prior to intervention – helps us to both protect vulnerable patients but also comply with standard medico-legal procedure.
Diagnosing – or predicting – OSD
“Pre-operative evaluation of patients for dry eye is fast, simple, and inexpensive: observe eyelids and blink rate; ask about symptoms; and – most critically – stain the ocular surface.” – Maurizio Rolando
“Just watch the patient: how often do they blink? Frequent blinkers have a low tear break-up time – you know that even before you put the fluorescein in.” – Sheraz Daya
“You should give Schirmer’s to a patient at least once – you have to understand if they can react.” – Maurizio Rolando
Top tip: Check for contacts
“Use of contact lenses is a red flag – always evaluate the ocular surface in more detail for those patients.” – Sheraz Daya
“Tear production is a reflex reaction to evaporation-induced temperature falls detected by the temperature sensor in the cornea. Contact lens wearers tend to be less temperature-sensitive, and hence produce progressively less tear flow.” – Maurizio Rolando
“Contact lens wearers blink less often, and then only partially; fluorescein stain follows a line – everything above it is clear, everything below is stained.” – Sheraz Daya
“All my serious dry eye cases get steroids as a first-line approach, to manage the inflammation. That’s very important, because inflammation depresses tear production.” – Maurizio Rolando
“In less serious cases, managing ocular inflammation is like steering a ship – if you turn too quickly, you’ll tip over! Better to drift carefully in the right direction: start on artificial tears, and only move to steroids if necessary.” – Sheraz Daya
“Consider preservative-free pre-operative steroids to enhance post-surgical healing.” – Ingeborg Stalmans
“Avoid preserved NSAID formulations – they can lead to extreme reactions, including corneal melt. Better to use higher doses of preservative-free steroids.” – Dawn Sim
“The ocular surface naturally produces endogenous cortisone to down-regulate reactions to environmental irritants – why not support this with topical hydrocortisone? It is relatively mild and is rapidly metabolized into non-active form.” – Maurizio Rolando
Effective dry eye management, both pre-surgery and post-surgery, significantly improves the chances of a successful outcome. This reality applies to the entire spectrum of patients likely to consult an ophthalmic surgeon – not least LASIK candidates, glaucoma patients and retinal surgery candidates. What key points should inform our patient management strategy?
Checks and choices
“There are five things to assess in any patient with ocular surface problems: inflammation, tear film instability, epithelial damage, lid problems, and nerve problems.” – Maurizio Rolando
“I advise pre-surgical identification of patients at risk of OSD, and administration of ocular lubricants to every patient post-injection.” – Dawn Sim
“Less is more... multi-therapy can lead to inflammation-induced IOP elevation and can impact surgical outcomes. Switching (and even reducing) the number of eye drops to eliminate pro-inflammatory agents such as preservatives and to improve compliance can result in a better IOP control, sometimes avoiding the need for surgery. Safer surgical options nowadays facilitate the choice for earlier surgery.” – Ingeborg Stalmans
Premium tears, not pretend tears
“It’s not true that a more severe dry eye should have more viscous artificial tears.” – Maurizio Rolando
“Cellulose-containing artificial tears adhere to the ocular surface and thereby protect the epithelium – but use lower concentrations to avoid blurred vision.” – Maurizio Rolando
“Hyaluronic acid-containing artificial tears are also protective, but are less viscoelastic, so they give the patient a better blink; furthermore, they can be sufficient in themselves to stabilize the ocular surface. Multiple action tear substitutes (MATS) combine the viscosity of hyaluronic acid with the protection of cellulose – and protect the ocular surface against the different conditions experienced in a broad range of lifestyles.” – Maurizio Rolando
LASIK:
“In high-performance surgery – multifocals, trifocals, and similar – you must ensure the ocular surface is optimal.” – Sheraz Daya
“Sometimes, with standard OSD management, your post-LASIK patient will come back with worse dry eye than before the surgery, and with a wound that’s melting down.” – Sheraz Daya
Retina:
“Intravitreal injections require regular administration to be effective, but eyedrop-associated ocular surface discomfort contributes to increased non-compliance rates in patients with diabetic retinopathy.” – Dawn Sim
“We assess the cornea pre-injection, to identify at-risk patients, and protect the ocular surface by administering lubricants post-injection. This actually gives the patient a better overall injection experience.” – Dawn Sim
Glaucoma:
“Everyone knows that preservative-containing eye drops are bad for the ocular surface, but rather than thinking ahead, we often start treating a chronic condition with preserved eyedrops, even though the toxic effect is cumulative.” – Ingeborg Stalmans
“The number of eye drops and the duration of treatment correlates with conjunctival infiltration of inflammatory cells and fibroblasts, which promote post-operative inflammation and scarring – if you want surgical success, you must take better care of the ocular surface.” – Ingeborg Stalmans
“Eye-drop preservatives may cause anterior chamber inflammation, which could impair trabecular meshwork function – a possible mechanism for inflammation-induced increases in IOP.” – Ingeborg Stalmans
The result of our expert forum provides the ophthalmology community with key guidance, as follows:
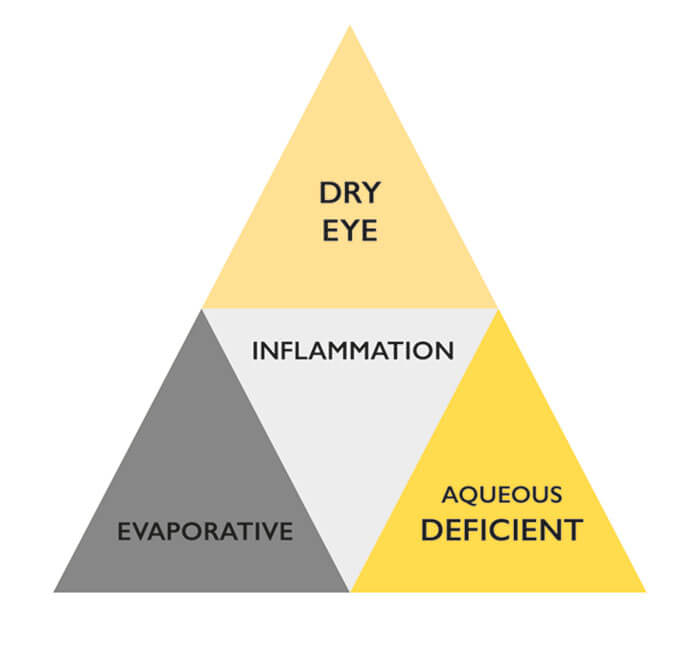
Firstly, note that OSD is a significant and growing problem, and that although not all OSD cases are the same, they all share key aspects of a multifactorial etiology – not least, inflammation. As Sheraz Daya says: “Both under-productive dry eye and evaporative dry eye are driven by an inflammatory component. Assessing its magnitude and cause is essential for long-term management of OSD.”
Secondly, be aware of the very significant pool of patients with sub-clinical dry eye; any given clinical intervention could be enough to push these patients over the edge into more serious OSD. “Remember,” says Maurizio Rolando, “dry eye may be just around the corner – and it will influence patient perceptions, because they will blame their OSD on your surgery.” But forewarned is forearmed: at-risk patients can be identified by careful application of standard diagnostic procedures. These include blink-rate assessment, Schirmer’s with anesthetic to measure tear-flow, and vital stains – notably, the fluorescein stain as modulated by a yellow filter.
Thirdly, as a consequence of careful diagnostic triage, pre-disposed patients may be managed so as to protect and stabilize the ocular surface. Broad strategies include: avoiding eye-drop formulations that contain preservatives or particularly problematic active ingredients (such as NSAIDs); reducing the number of eye drops; and applying lubricant after interventions, such as intravitreal injections. As Ingeborg Stalmans puts it: “If you want surgical success, take care of the ocular surface.”
Finally, be aware that the issues outlined in this supplement apply to a very broad spectrum of patients – the advice given here is therefore pertinent to a correspondingly broad range of ophthalmologists. Not everybody appreciates this: “The problem with retinal specialists is that we tend to see the cornea only as a window to our area of interest,” says Dawn Sim. “We don’t always pay attention to the ocular surface, but it makes such a difference for patients.” Ingeborg Stalmans agrees: “Glaucoma specialists are no different. We know preservatives are bad, but we don’t always act like we know it in the clinic.” And Sheraz Daya, in the LASIK field, is well aware of the benefits of careful pre- and post-surgical management of the ocular surface. The last word goes to Maurizio Rolando: “Think dry eye – before the patient does.”

References
- JAP Gomes, et al., “TFOS DEWS II Iatrogenic report”, Ocul Surf, 15, 511-538 (2017). JP Craig, et al., “TFOS DEWS II Definition and Classification Report”, Ocul Surf, 15, 276-283 (2017).
