IOP is known to fluctuate over the course of the day and under different physiological conditions, meaning that single office measurements do not represent the full story. “From discussion with ophthalmologists it is clear that there is much dissatisfaction with the current method to quantify IOP, and there is a need to monitor over at least a 24-hour period to record the IOP profile during sleeping and normal day activities,” says Ahmed Elsheikh, Professor of Biomaterial Mechanics at Liverpool University, Liverpool, UK.
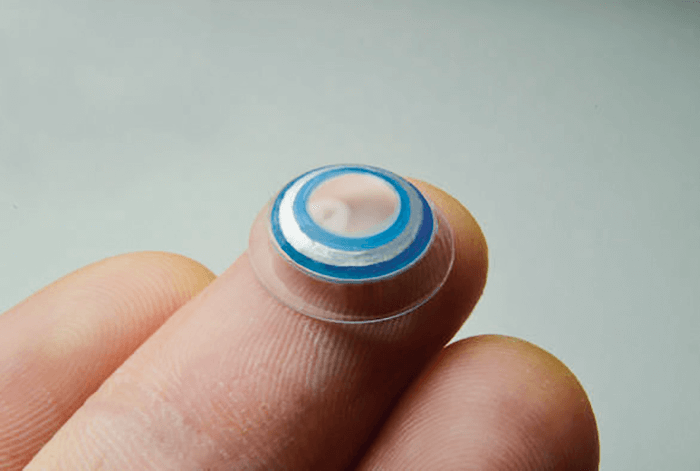
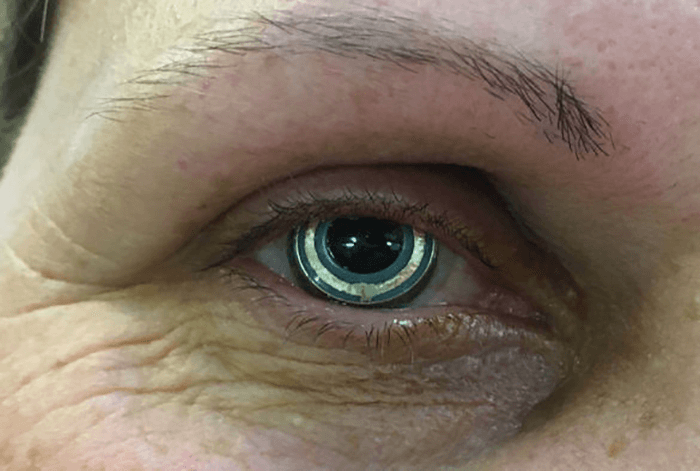
But that’s easier said than done: “Efforts to address the challenge of continuously monitoring IOP have been going on for more than 40 years, and we still don’t have a reliable clinical solution,” explains Elsheikh. “It is a difficult challenge because the device needs to measure IOP non-invasively, as well as deal with the continuous movement of the eye and eyelids, and transfer the measurements wirelessly.” Undeterred by the challenge, Elsheikh and his team have been working on a solution since 2008: a low-cost contact lens tonometer (1). The hydrogel contact lens (Figure 1) contains a patented pressure sensor built into a ‘bridge’ portion of the contact lens that can factor in mechanical behavior of the cornea and the sclera. It also includes a telemetry system that transmits IOP measurements to an external instrument. The sensor lies on the back portion of the lens, and sits upon the surface of the eye; IOP measurements are collected during reactive deformation in the device, when the subject’s eyes are closed during blinking or sleeping (2). According to Elsheikh, their device differs from the commercially available Triggerfish smart contact lens through its method of operation. “Our device relies on corneal applanation whereas the Triggerfish relies on tracing topography changes,” he explains. “Another main difference is that our device provides profiles of IOP changes in actual pressure values (mmHg) that clinicians can directly relate to and use in practice; the triggerfish provides IOP changes in arbitrary units.” But does their device work? In a recent pilot study conducted at St Paul’s Eye Unit (Liverpool, UK) and Moorfields (London, UK), 12 volunteers wore the contact lens for one hour rather than 24, during which time the researchers found that the device could track IOP changes whilst causing minimal discomfort (2). Further clinical studies are on the horizon, along with refinement of manufacturing techniques in a bid to commercialize the device.
References
- University of Liverpool. “Clinical study success for novel contact lens device to improve glaucoma treatment”. Available at: http://bit.ly/2i50YKg. Accessed October 25, 2017. Google patents. “Device for monitoring intraocular pressure US 20130184554 A1”. Available at: http://bit.ly/2gL5tND. Accessed October 26, 2017.
