Since 2010, the “prevention of macular edema after cataract surgery” (PREMED) study has been running across 12 European centers to address the lack of consensus on the most effective anti-inflammatory regimen. Even the AAO and the ASCRS have published opposing views on the subject:
- In their 2015 report, the AAO wrote: “There is a lack of level 1 evidence that supports the long-term visual benefit of non-steroidal anti-inflammatory therapy when applied solely or in combination with corticosteroid therapy” (1).
- A 2016 report from the ASCRS Cataract Clinical Committee and the American Glaucoma Society concluded: “Whether used alone, synergistically with steroids, or for specific high-risk eyes, the efficacy of NSAIDs is compelling” (2).
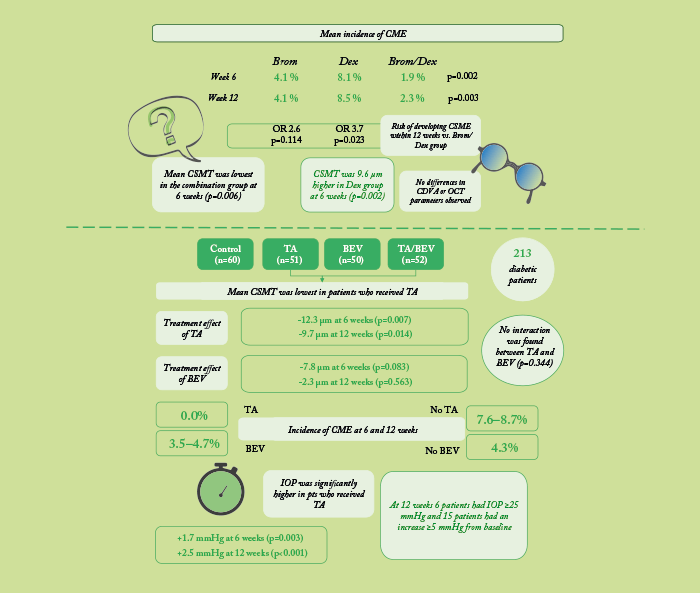
So what is the best approach? On October 8, 2017, full results of the PREMED study – which included over 1,000 patients with and without diabetes who underwent phacoemulsification cataract surgery – were presented at the ESCRS annual meeting in Lisbon, Portugal, by Rudy Nuijts and Laura Wielders of Maastricht University Medical Center in The Netherlands. Nuijts presented data from 914 patients without diabetes who were randomized to topical bromfenac, topical dexamethasone, or a combination of both. Wielders presented data from 213 patients with diabetes who were randomized to receive intravitreal triamcinolone acetonide, bevacizumab, or a combination of both; all diabetic patients also received topical bromfenac and dexamethasone. Patients were followed up postoperatively at six and 12 weeks. We summarize the studies and key results in the infographic above. The main conclusions? For non-diabetic patients, a combination regimen of topical bromfenac (0.09%) and dexamethasone (0.1%) was associated with a lower risk of developing CME after cataract surgery (3). In patients with diabetes, both a single 40 mg triamcinolone injection, and the bromfenac and dexamethasone regimen, were found to be effective, with intravitreal bevacizumab having no significant effect (4). However, as IOP was significantly increased in patients who had received triamcinolone, Wielders concluded, “the risk of developing CME should be carefully weighed against the risk of developing an increased IOP” (4). Nuijts commented that the findings from the study offer “the foundation to draw up concrete evidence-based recommendations to prevent the occurrence of CME after cataract surgery in patients with and without diabetes” (3).
References
- SJ Kim et al., “Topical nonsteroidal anti-inflammatory drugs and cataract surgery: a report by the American Academy of Ophthalmology”, Ophthalmology, 122, 2159–2168 (2015). PMID: 26123091. RS Hoffman et al., “Cataract surgery and non-steroidal anti-inflammatory drugs”, J Cataract Refract Surg, 42, 1368–1379 (2016). PMID: 27697257. R Nuijts. “The PREMED Study: CME prophylaxis”. Presentation at the European Society of Cataract and Refractive Surgeons, October 8, 2017; Lisbon, Portugal. L Wielders. “Can perioperative treatments decrease the risk of CME in diabetics?” Presentation at the European Society of Cataract and Refractive Surgeons, October 8, 2017; Lisbon, Portugal.
