The last five years has seen the rise of MIGS – in terms of the “micro invasive” approach, and the devices that go with them. The information that’s currently out there (and there’s little beyond manufacturer-sponsored studies at the moment) suggests that, relative to interventions like trabeculectomy or tube shunts and valves, it’s a relatively safe approach to moderately lower IOP. MIGS, however, is not a panacea. There are other options, such as selective laser trabeculotomy (SLT), to control a patient’s IOP that are often worth pursuing first, and it’s definitely worth bearing in mind that the MIGS umbrella encompasses many unique devices, with unique implantation techniques, unique learning curves – and also unique issues. Every ophthalmology department has a laser – and it’s more useful than you might think. I want to tell you about how I use YAG and Argon lasers to fix some of the issues that can arise with MIGS devices – and how this can be achieved in the clinic, rather than requiring a return to the operating theater for surgical stent revision.
Optimizing outcomes
There can be a big difference between what you can visualize with pre-operative gonioscopy at the slit lamp and what you can see through a gonio lens during surgery. First, patients can be more mobile on the operating table due to anxiety. Second, and most importantly, it’s about optics and lighting. It’s easy to get an adequate gonio view at the slit lamp and clearly define the corneal light wedge and Schlemm’s canal. Intraoperative microscopy is always coaxial, meaning you can’t illuminate obliquely, which makes it harder to identify exactly where you want to place the stent. Normally or heavily pigmented angle structures might be adequately visible under these conditions – but this isn’t the case with very pale angle structures. When I come across this during slit lamp gonioscopy, I use an Argon laser to “mark” the meshwork in the nasal quadrant (in three areas usually) meaning I just have to insert my stent on the mark during surgery. Anecdotally, because the region has also been photocoagulated by the laser, it also reduces the hemorrhage that sometimes occurs as the sharp tip of iStent enters the angle.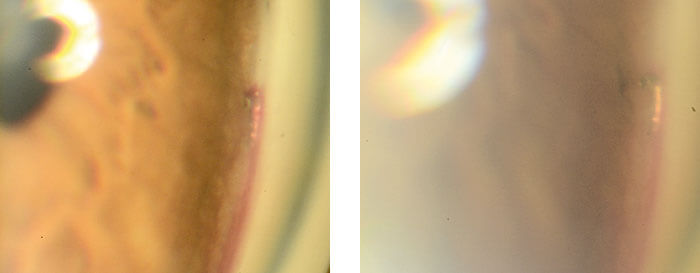
Treatment complications
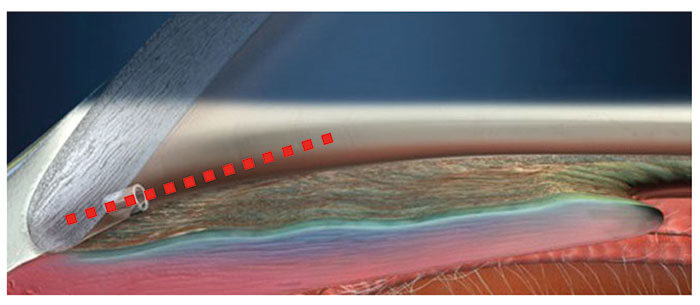
Anything with a lumen in the eye can get blocked, and MIGS devices are no exception. Be it blood, fibrous or inflammatory membrane – or even iris tissue – it’s important to note that, rather than performing revision surgery, you can use a few shots of a YAG laser to clear the blockages. There are a number of risk factors for stent blockage – and a lot of it comes down to ocular anatomy. Let’s take the iStent (Glaukos) as an example (Figure 1). If you’re placing an iStent into an eye that’s slightly shallow or the angle is not wide open, the iris is, by definition, quite close to the stent. If your patient’s iris is a bit high, or for some reason, someone’s dilated the pupil, the pupil can plug the lumen of the stent. The iStent lumen can rotate anteriorly or posteriorly whilst still perfectly seated in the canal. If you leave the stent pointing to the cornea it should never block. However, leaving the lumen pointing below the iris plane (or if your stent rotates) results in an increased risk of problems. These risks increase in shallow eyes and eyes with narrow angles – there’s simply less margin for error. A recent review of the iStent literature (1) found that the rates of occurrence of malpositioning and occlusion that necessitated surgical intervention (YAG laser, tissue plasminogen activator [tPA], or stent revision) ranged from 4.5–11.3 percent – and was cited as the most common complication across the studies. But irrespective of whether the iStent has become malpositioned and blocked because of anatomy, poor surgical technique, postoperative movement or plain bad luck, it can be fixed with the YAG laser in just a few shots – in the clinic, rather than the operating theater. After all, prevention is better than cure.1991 Optotek founded
1996 R&D and production of optoelectronic products
1997 First laser systems for dermatology produced
1999 First ophthalmic laser systems
1999 OEM YAG laser system and Q-Las photodisruptor launched
2004 HawkEye portable slit lamp launched
2007 Acquired by OptoPol technologies
2008 LacriMax, OptoYag, OptoSLT, OptoYAG&SLT launched
2009 OptoPol technologies acquired by Canon Inc.
2014 OEM YAG laser system and OEM combined laser system launched
2015 New LacriMax launched
2016 OptoSLT nano launched – the first DPSS laser for SLT
So once again, the approaches I take to fix these situations are:
- Clear any blockage – I use my Optotek YAG laser to quickly clear the stent, and
- If the iris is being chafed or snagged, I use an Argon laser to contract the iris out of the way (behind the stent), so there’s no longer any contact.
Box 1. Treatment of blocked iStent
- Blood in lumen. Wait, try steroid drops, YAG laser to clear if no response at 2 weeks
- Inflammatory membrane. Wait, steroid drops, tPA injection in anterior chamber at 1 week, YAG laser to clear at 2 weeks
- Iris blockage. Don’t wait. Try Pilocarpine - see 1 hours. Argon laser iridoplasty around the tip to contract. YAG laser to clear any remaining strands
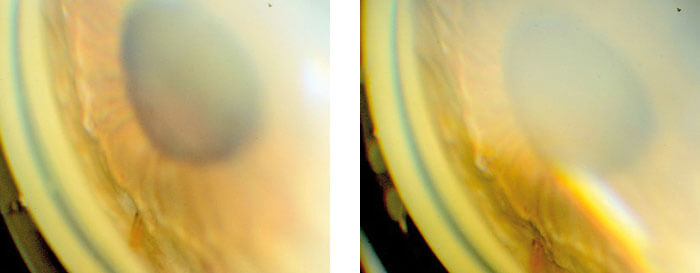
It’s a similar story with Xen (Allergan): it’s a longer stent, and it can go much further into the anterior chamber. Problems can arise with Xen if it’s inserted too posteriorly (below the trabecular meshwork, closer to the iris), or even if it’s inserted at the correct angle landmark, but the stent extends too far into the anterior chamber – resulting in iris block in the mid-periphery. The emphasis has to be getting this right the first time by using an intraoperative gonio lens to place the Xen rather than the unguided/ “blind” Xen insertion approach some surgeons take. Having said that, if iris block or iris chafing occurs, this can result in persistent uveitis and inflammation, so it needs to be dealt with promptly (Figure 2). Again, the laser can help. If there’s hemorrhage, the best course of action is to use the YAG laser to clear the stent early – it’s important to get aqueous flowing early though the Xen. If you wait for the hemorrhage to clear naturally then you risk a situation of no flow down the tube and conjunctival healing/scarring and early bleb failure. It’s the same with inflammatory membranes – you really do need early flow to protect the bleb. In essence, the message is: use the laser, don’t wait for the medication to work.
References
- SR Wellik, EA Dale, “A review of the iStent(®) trabecular micro-bypass stent: safety and efficacy”, Clin Ophthalmol, 9, 677–684 (2017). PMID: 25931808.
