Many attempts have been made over the years to help reduce the occurrence of posterior capsule opacification (PCO) after cataract surgery. Lens epithelial cells (LECs) are the target: anything that inhibits their migration to (and proliferation on) the posterior capsule will help. Square-edged IOLs were a great step forward; they formed a physical barrier to LEC migration – but alas, given enough time, that barrier will be breached. Over the years, a number of approaches have been made, including capsular polishing, the bag-in-the-lens procedure, and leaving the capsular bag open. The latter seems to work… but people have always speculated why?
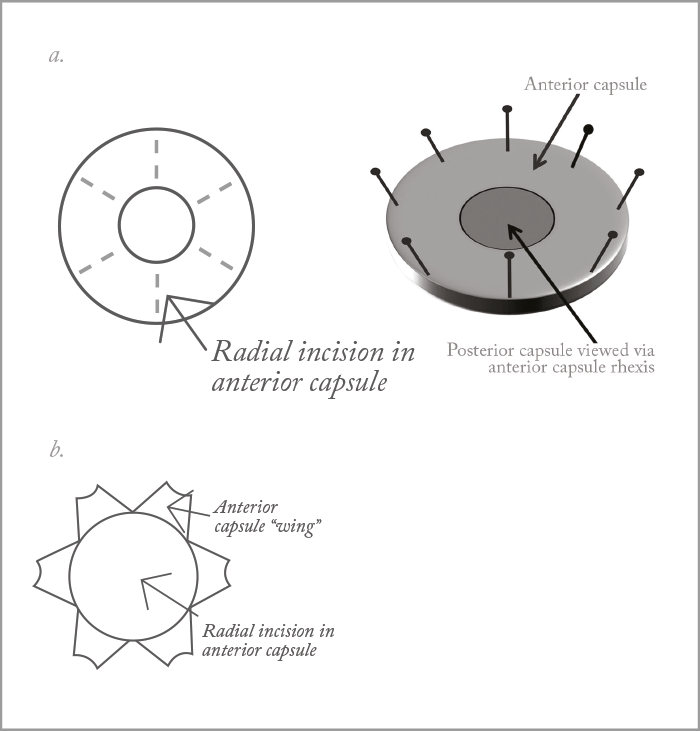
The hypothesis is this: unlike standard IOLs where the capsular bag “shrinkwraps” around the IOL, if the bag is open, it’s subject to greater irrigation by the aqueous humor, which washes away (or at least dilutes) the cytokines that promote LEC migration and proliferation. Eldred et al. (1) decided to test that hypothesis using human lens cell and tissue culture experiments. Using donor eyes, with lenses hydrodissected out through a small capsulorhexis, the researchers created a “closed bag” preparation (see Figure 1a) that was placed in cell culture. To mimic the dilution of growth factors, they simply cultured the tissue preparation in different volumes of culture media (1.5 and 6 mL) and measured the proportion of the posterior capsule that was covered by cells. Volume mattered: after only 8 days of culture, posterior capsule cell cover was significantly lower in the 6 mL group than the 1.5 mL group. The experiment was repeated with an “open bag” preparation (see Figure 1b): posterior capsule cell cover was sparse in the 1.5 mL group, and non-existent in the 6.0 mL group, lending further credence to their hypothesis.
But if cytokines are at play, which ones are they? The team analyzed the media collected from the closed bag preparations: 24 cytokines were detectable in both the 1.5 mL and 6 mL cultures, but only nine were significantly reduced in the 6 mL culture (above and beyond that of simple fourfold dilution from the 1.5 mL culture). These were IL-8, IL-15, IL-12(p70), MCP-1, MIP-1β, IL-1ra, IL-10, IP-10 and VEGF. There’s a human fetal lens epithelium cell line available, FHL 124, so the researchers’ next step was to assess the effect of each cytokine on the migration of FHL 124 cells. Ultimately, VEGF was identified as the likely culprit, as both the VEGFR-1 and -2 receptors are expressed in these cells, and their migration was significantly reduced when the VEGF-receptor antagonist, axitinib, was added to the culture medium. Further, axitinib reduced cell cover in their initial “closed bag” model – suggesting that VEGF is a survival or growth factor for human LECs. So it looks like we have an explanation for why open-bag IOL use is associated with lower PCO rates – and it raises the question of whether the application of perioperative VEGF inhibitors to the capsular bag (perhaps as an IOL coating) might be another way of keeping those pesky LECs at bay.
References
- JA Eldred et al, “Growth factor restriction impedes progression of wound healing following cataract surgery: identification of VEGF as a putative therapeutic target”, Sci Rep, 6, 24453 (2016). PMID: 27076230.
