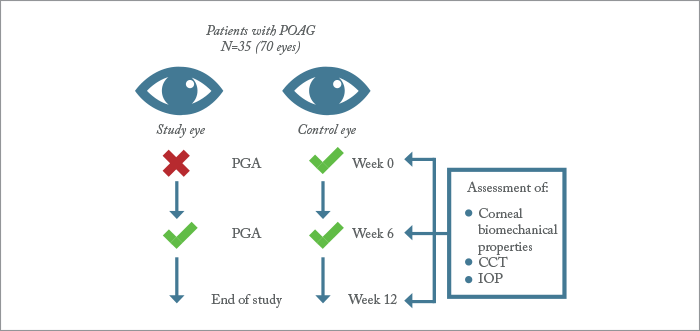
The relationship between intraocular pressure (IOP), central corneal thickness (CCT) and the manifestation of glaucoma is a complex one. It’s long been known that you need to take into account CCT when measuring patients’ IOP; the smaller a patient’s CCT, the greater their chance of developing primary open-angle glaucoma (POAG) (1),(2). But with research showing topical anti-glaucoma therapies can thin patients’ corneas (3),(4), the question people are asking is: how might prostaglandin analog (PGA) treatment affect the accuracy of IOP monitoring with Goldmann Applanation Tonometry (GAT)? A Montreal-based team of researchers decided to investigate (5). They recruited 35 patients (70 eyes) with POAG who were on chronic topical PGA therapy (mean treatment duration, 3.99 years) into a prospective, 12-week interventional case-control study. Each patient ceased PGA therapy for a six-week period in one eye (the better, “study eye”), before recommencing therapy afterwards (Figure 1). The contralateral eye continued to receive therapy throughout the study, and acted as control.
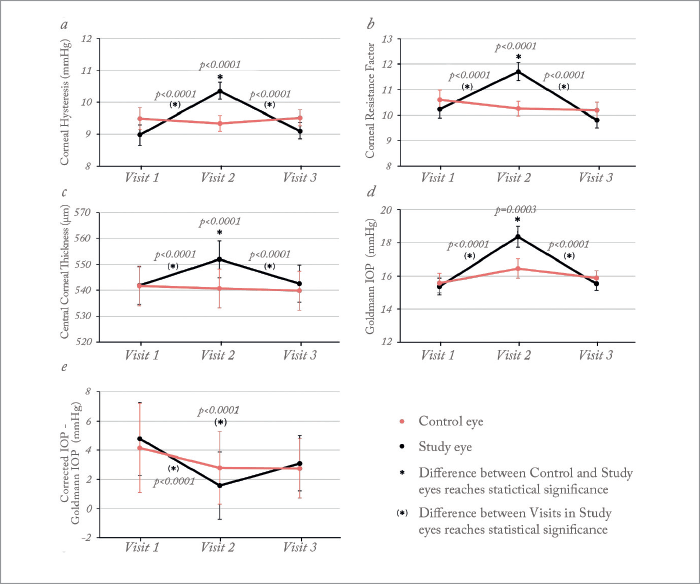
They assessed patients’ corneal biomechanical properties, CCT and IOP in both eyes at baseline, at the end of the 6 week treatment cessation period, and at the conclusion of the study, at 12 weeks. CCT was measured by ultrasound pachymetry; corneal biomechanical parameters were measured using the Ocular Response Analyser (ORA, Reichert), and IOP was measured in two ways: using GAT (IOPGAT), and with ORA to generate a “corneal-compensated” IOP measurement (IOPCC), that should be less affected by changes in the properties of the cornea – like CCT (6). This enabled them to calculate “IOP bias” (IOPCC—IOPGAT). Positive bias values would mean GAT underestimates IOP (relative to the values provided by ORA), whereas negative bias values would suggest the opposite. What they found was that chronic PGA therapy induces reversible changes in CCT and corneal biomechanical parameters. Six weeks of no therapy in the study eye led to significant increases in corneal hysteresis (CH), corneal resistance factor (in crude terms, how “stiff” the cornea is), and CCT. These changes were reversible, though – at 12 weeks (after having recommenced topical PGA therapy for six weeks) baseline values were restored (Figure 2). In other words, PGA therapy appears to “soften” the biomechanical properties of the cornea. Crucially, the team found that GAT significantly underestimates IOP in patients when they receive PGAs: relative to baseline values, at week six, IOPGAT was significantly increased, and IOP bias was significantly decreased (Figure 2). During the study, the six-week interruption in PGA therapy in study eyes reduced GAT IOP underestimation by an average of 3.2±0.6 mmHg. According to the study authors, the findings “raise concern over the accuracy of IOP measurements in patients under chronic PGA therapy,” and called for “additional caution when assessing the effectiveness of [topical] IOP lowering [therapy], especially in patients with more advanced glaucoma, which in itself tends to be associated with lower CH.”
It’s been a very busy few weeks in the ophthalmic business space, with several high-profile FDA approvals and companies such as Zeiss, Santen and AcuFocus making important announcements. To read our exclusive online-only coverage, visit: top.txp.to/issues/0716/206
References
- MO Gordon et al., "The ocular hypertension treatment study: baseline factors that predict the onset of primary open-angle glaucoma", Arch Ophthalmol, 120, 714–720 (2002). PMID: 12049575. MC Leske et al., “Predictors of long-term progression in the early manifest glaucoma trial”, Ophthalmol, 114, 1965–1972 (2007). PMID: 17628686. Y Maruyama et al., “Effect of long-term topical prostaglandin therapy on central corneal thickness”, J Ocul Pharmacol Ther, 30, 440–444 (2014). PMID: 24738848. WA Schrems et al., “The effect of long-term antiglaucomatous drug administration on central corneal thickness”, J Glaucoma, 25, 274–280 (2016). PMID: 25383467. R Meda et al., “The impact of chronic use of prostaglandin analogues on the biomechanical properties of the cornea in patients with primary open-angle glaucoma”, Br J Ophthalmol, 2016 [Epub ahead of print]. PMID: 27162226. N Terai et al., “Identification of biomechanical properties of the cornea: The Ocular Response Analyzer”, Curr Eye Res, 37, 553–562. PMID: 22559332.
