This article has been initiated and funded by Santen
In December 2019, an acute respiratory syndrome caused by a novel coronavirus emerged from China and began spreading across the world. In addition to rare cases of COVID-19-related conjunctivitis, the pandemic could have wider implications for patients with existing ocular problems, in particular dry eye disease. Stefano Barabino, Head of the Ocular Surface Center at the Sacco Hospital, Milan, Italy, tells us more.
How is the COVID-19 pandemic affecting patients suffering from dry eye disease?
The pandemic has profoundly changed our everyday lives. During lockdown, opportunities for venturing outside were significantly limited; in Italy, we weren’t even allowed to go outside for walks or exercise, and in other countries there were strict time limits imposed. This has been a real problem for patients with dry eye disease, as low humidity and restricted airflow indoors can induce or exacerbate the condition. Low humidity means a higher evaporation of tears from the ocular surface, which in turn leads to more flare ups of dry eye disease.
Another concern is that a COVID-19 lockdown can prevent patients’ eye check-ups and limit their access to treatment for dry eye and other ophthalmic conditions.
Do other aspects of the pandemic affect dry eye patients?
Home confinement, e-learning and working from home means we’re spending more time looking at screens, and this has a significant impact on eye health. Typically, each eye has a tear film that is spread across its surface each time we blink. If the integrity of the tear film is high, the quality of vision will be excellent. A break in the tear film can reduce vision quality and cause feelings of grittiness and burning. This is due to the evaporation of the tear film, so blinking is essential for the proper function and feel of the ocular surface.
Sitting in front of a screen, we simply do not blink enough. Studies have shown the average number of blinks decreases from about 18 per minute in normal conditions to three or four per minute while watching a screen (1). Moreover, when we blink while screen watching, that blink is not as forceful or complete. This combination of reduced frequency and intensity of blinks during screen time increases the risk of inducing or exacerbating dry eye disease.
How have you been managing your dry eye patients during the pandemic?
The critical points are to keep in touch with your patients, even if in-person eye checks aren’t possible, and to continue their current treatment. If they use substitute tears or topical anti-inflammatory treatments, they should continue to do so. In cases where ongoing steroid use is causing problems, the patient can taper down the number of applications. We may also recommend that patients stay in a high-humidity environment, which can usually be achieved with a home humidifier, and increase the number of artificial tear applications and screen breaks to increase their blink rate.
How will your practice adapt to the “new normal”?
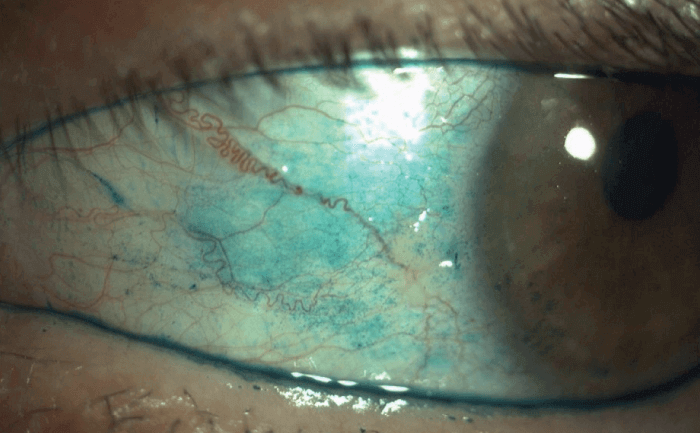
Along with all the protocols to block viral transmission, we will probably have fewer opportunities to examine our dry eye patients in person for many months to come. Ultimately, we will need to migrate to new technologies, such as digital photography, to help compensate for this. For example, conjunctival hyperemia is a sign of increased inflammation that can be diagnosed fairly easily from a photograph. We could even consider asking patients to self-administer vital stains such as a fluorescein and lissamine green (2) (see Figure 1) and send us high-definition pictures to aid diagnosis.
New technologies can help, but they cannot replace a good bedside manner or communicating with compassion. Patients tend to rely on these interactions for a sense of well-being. It is paramount to have some reassuring words for our patients, to let them know we are caring for them, even if we are not able to see them in person.
How do you reassure patients and increase motivation, compliance and adherence to treatment plans?
For dry eye patients, I describe the chronic nature of their disease and explain that changes are possible during its course and that symptoms can worsen and improve. If the dry eye is accompanied by Meibomian gland dysfunction, it’s very important to use artificial tears and steroids, with tetracycline ointment applied to the eyelid.
Lid hygiene is also fundamental, along with regular application of hot compresses. It should be done every day, and some studies show that lid hygiene can increase the breakup time of the tear film (3). These are important factors for patients to understand, along with our commitment to their care and our ongoing availability for consultation and necessary treatment.
Date of preparation: July 2020. NP-FOTE-EMEA-0151
- S Patel et al. “Effect of visual display unit use on blink rate and tear stability,” Optometry and Vision Science, 68, 888 (1991). PMID: 1766652.
- S Yang et al. “The use of conjunctival staining to measure ocular surface inflammation in patients with dry eye,” Cornea, 38, 698 (2019). PMID: 30844839.
- M Okura et al., "New eye cleansing product improves makeup-related ocular problems", J Ophthalmol (2015). PMID: 26347812.
