- Corneal inlays for presbyopia may be associated with drawbacks including compromised contrast sensitivity and degraded stereoscopic acuity
- These issues are largely a consequence of the diffraction of light through the thousands of micropores required to allow nutrient diffusion across the implant
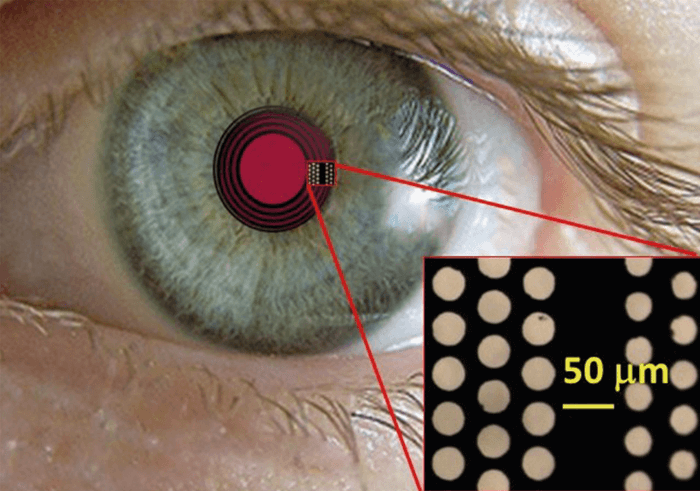
- By exploiting the photon sieve concept, we have created the diffractive corneal inlay (DCI), a device that diffracts light by design
- The DCI is the basis for a corneal inlay that not only avoids issues of degraded contrast sensitivity and stereoscopic acuity, but also corrects presbyopia and higher order aberrations on a personalized basis.
What are the surgical options for presbyopes who don’t want glasses or contact lenses? One possibility is to implant a corneal inlay. These devices are intended to increase depth of focus, and thus improve near vision without significantly affecting distance vision. The inlay procedure is fast and simple: using a femtosecond laser, the surgeon creates an intracorneal pocket of appropriate position and dimensions, and inserts the inlay. Recovery is usually complete in one or two days. At present, corneal inlays are available in two forms: the refractive inlay and the small aperture corneal inlay (SACI), as represented by the Kamra product. Refractive inlays are very simple, being no more than small lenticules that can locally modify corneal power and/or curvature – and thereby modulate depth of focus – when correctly positioned. The SACI, by contrast, is an opaque disc with thousands of micro-pores and one larger central aperture. The central aperture exploits the pinhole effect so as to increase the depth of focus of the eye. Implantation of a solid disc, however, would block the flow of nutrients to cells of the corneal stroma; to prevent this, the SACI must be made permeable. Hence the SACI micro-pores – more than 8,000 of them, in a size range of 5–11 µm diameter. Unfortunately, although SACI implantation can result in good clinical outcomes, there are some drawbacks. First of all, only about 20 percent of the incident light passes through the disc's central aperture. Secondly, as much as five percent of incident light is diffracted by the disc's pores. The net effect of these handicaps is that the improvement in near vision provided by a SACI procedure comes at a significant cost to contrast sensitivity. For this reason, patients only ever receive SACI in one – the non-dominant– eye, never both, the idea being that the non-SACI eye will compensate for the compromised vision in the SACI eye. But this monocular approach results in the additional issue of degraded stereoscopic acuity (1)! Might there be a better way?
Seeing the light
Of course, SACI manufacturers are aware of the limitations outlined above, and have investigated various mitigating strategies. In particular, they have tried to minimize the diffractive effect of the micro-pores by decreasing their diameter and distributing them randomly on the disc. It occurred to my colleagues and I, however, that the pores could be turned to our (and patients’) advantage. Our inspiration came from the photon sieve – a device that uses an array of pinholes to focus light by means of diffraction and interference, thus capitalizing on the very features that SACI manufacturers were trying to eliminate. Another great benefit of the photon sieve is that its optical characteristics can be modulated by varying the size of the pinholes and the pattern of their distribution – suggesting that devices based on the photon sieve concept could be customized for a variety of specific applications. We knew that photon sieves had already been applied in X-ray microscopy, and used as alternatives to lenses or mirrors in telescopes, so why not try them in vision correction? It seemed like a relatively simple proposition to test; all we needed to do was distribute the pores in a precisely designed pattern, and a SACI-type disc should be turned into a diffractive lens that brings near objects into focus. So we set out to merge the photon sieve and the SACI pinhole-effect concept to develop a novel corneal implant – the diffractive corneal inlay (DCI: Figure 1). The DCI’s disc pores would not just permit the flow of nutrients, but also deliberately and precisely diffract light to create a new focus for near distance. Furthermore, we expected that by optimizing the spatial distribution of the pores, we would be able to vary the relative intensity between near and far foci, and also correct higher order ocular aberrations. In this way, the DCI would be customizable according to specific patient need. In other words, our approach turns the diffractive effects of SACI from a disadvantage into a significant advantage, and in doing so provides an entirely new concept in corneal inlays! Theory was brought closer to practice by my colleagues and I in the Diffractive Optics Group, a multidisciplinary collaboration between a number of institutions. Together, we designed and performed a series of optical bench experiments to measure the polychromatic axial Point Spread Function (PSF) associated with different inlay designs, recording PSF along the optical axis under polychromatic illumination. In this way, we showed that the DCI’s performance was superior to that of the Kamra SACI (2). And given that the DCI permits passage of a very high proportion of incident light, it seems likely that patients could receive DCI implants in both eyes – avoiding yet another drawback of SACI.Looking ahead
In the near term, we are clearing the path to the clinic via two clinical investigations of the DCI device. One is aimed at testing the performance of soft contact lenses printed with a DCI array of pores. The other seeks to simulate the implant with a VAO visual simulator (Voptica, Murcia, Spain). At the same time, we are also investigating earlier-stage concepts, not least various transparent DCI designs that could be the basis of new types of multifocal IOLs. We are also investigating the application of novel materials for our device. To date, we have known that DCIs could be fabricated from the same material used for SACIs – namely, polyvinylidene fluoride. We believe, however, that we can improve on this aspect of corneal inlay devices too, and are currently engaged in proof-of-concept studies using graphene oxide. We chose graphene because its properties make it excellently suited for ocular implantation; for example, it is highly biocompatible with corneal tissue (3), has an ultrahigh refractive index, has linear optical absorption characteristics and can be manufactured in sheets thin enough to be implanted into the cornea without inducing refractive effects and even, can be held between two contact lenses in preclinical studies. We are very excited about this development.Personalizing refraction
But perhaps the most exciting feature of the DCI is its potential to be personalized according to the specific needs of each patient. The design of the device incorporates several free parameters that allow DCI customization according to requirements regarding reading/working distance and pupil size in different environmental conditions, and may even permit compensation for particular higher order aberrations. In practice, we would probably make each device in contact lens form initially, to confirm that it adequately corrects a given patient’s vision before proceeding to device manufacture and implantation. Of course, to bring this promising innovation to the market will require collaboration with industry, and we are actively inviting and pursuing such discussions. Walter Furlan is a Physicist in the Departmento de Óptica y Optometría y Ciencias de la Visión, Universitat de València, Spain. He would like to acknowledge his colleagues in the Diffractive Optics Group: Juan A. Monsoriu and Vicente Ferrando (Universitat Politécnica de València, Valencia, Spain); Laura Remón (Universidad de Zaragoza, Spain); Salvador García-Delpech and Patricia Udaondo (Aiken Clinic / Hospital La Fe de Valencia, Valencia).References
- WN Charman, "Developments in the correction of presbyopia II: surgical approaches", Ophthalmic Physiol Opt., 34,397-426 (2014). PMID: 24716827. WD Furlan, et al., "Diffractive corneal inlay for presbyopia", J. Biophotonics, 10, 1110-1114 (2017). PMID: 28635120. XW Tan, et al., "Application of graphene as candidate biomaterial for synthetic keratoprosthesis skirt", Invest Ophthalmol Vis Sci., 56, 6605 (2015). PMID: 26465888.
