Visual field assessment in infants is hard… and perimetry is incredibly difficult (1). But it’s important information to have when visual field disorders or strabismus is suspected, and it can help identify and exclude those cases where infants present with an “eye turn”, receive strabismus surgery, but actually have congenital hemianopia.
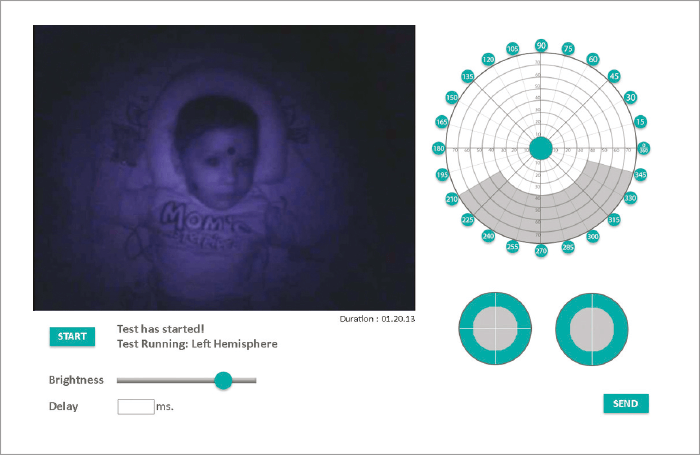
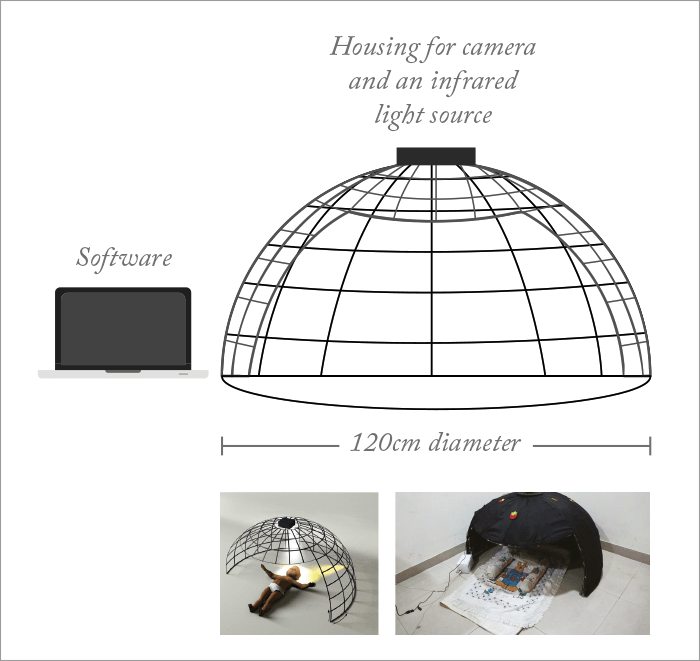
What if there was an easier way? The Pediatric Perimeter (1) is a hemispherical dome built out of steel rods to form 24 meridians (separated by 15°), that has an infrared (IR) camera at its apex, and is covered by black cloth (Figure 1). The infant is laid in the dome, and the infrared camera monitors their eye movements in response to LED stimulus patterns controlled by the clinician (Figure 1). Does it work? PremNandhini Satgunam of the L V Prasad Eye Institute in Hyderabad, India, and a lead member of the development team, explained that the perimeter has been used to successfully map visual field extent in both infants and toddlers. Further, it’s able to identify differences in the visual fields of infants with normal developmental milestones (NM) and those with developmental delay (DD). Five NM infants (mean age, 10.0±7.1 months) and 12 DD infants (mean age, 12.1±6.9 months) were assessed.
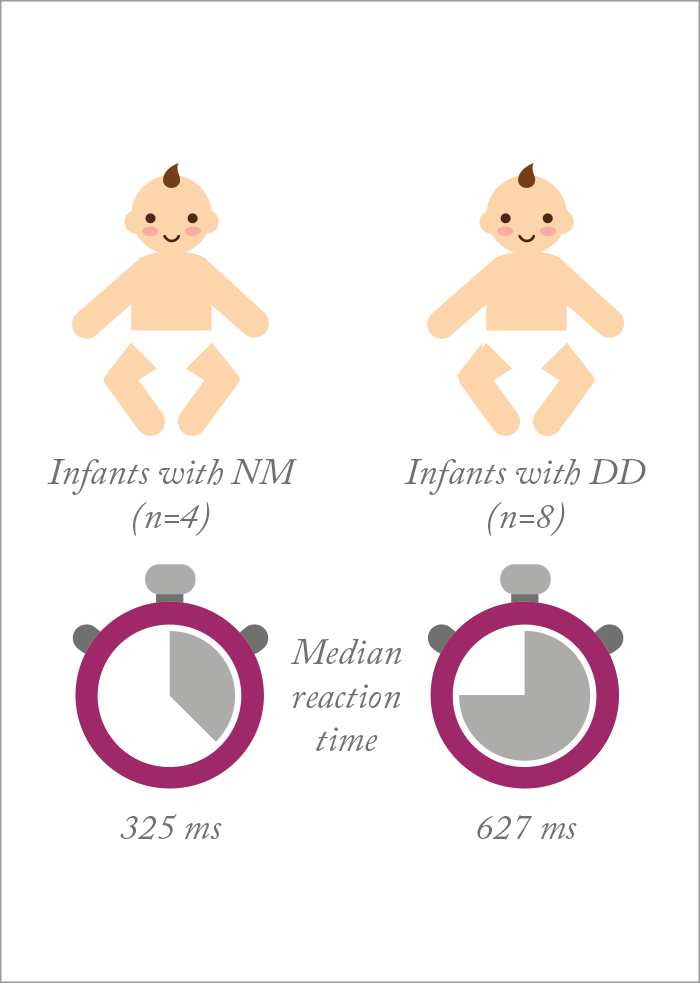
Although both groups displayed similar visual field extents, reaction times in DD infants were almost two times longer (Figure 2) – something that Satgunam ascribed to “potential processing delays in afferent, efferent, or both systems.” The team also showed preliminary findings that the visual field isopter may differ between infants with NM and DD, but Satgunam comments, “we need to do a lot more normative database measurement before we can say anything for certain.” If pediatric visual development is better understood, in both normal and DD children, as well as furthering knowledge to guide clinical practice, it may prevent unnecessary surgeries being performed on young children.
References
- V Dobson et al., “Visual field extent in children 3.5–30 months of age tested with a double-arc LED perimeter”, Vis Res, 38, 2743–2760 (1998). PMID: 9775323. P Satgunam et al., “Development of a novel device to measure visual fields in infants and toddlers”, IOVS 2016, 57, ARVO E-Abstract 5978-D0069.
