- A small subpopulation of patients experience poor outcomes after surgery
- Diagnostics and screening can help identify this problematic group
- Objective assessment of overall visual quality is a first step
- Topography and aberrometry further enhance outcomes
Eighty-five to 95 percent of the time, outcomes in cataract, refractive, and corneal inlay surgery are excellent (1,2). To help with that troublesome last 5-15 percent, we now have numerous advances in surgical technology, novel diagnostic equipment and improved patient screening at our disposal. Major improvements in laser technology through faster excimer lasers, more accurate eye trackers, and very precise femtosecond lasers mean that much of the potential for human error during surgery has been eliminated. It is now up to us to use the best diagnostic devices available to ensure that patients who are poor candidates do not slip through the safety net of proper screening. Here are my views on the diagnostic technologies that help to achieve optimal outcomes.
Refining pre-op, intra-op and post-op outcomes
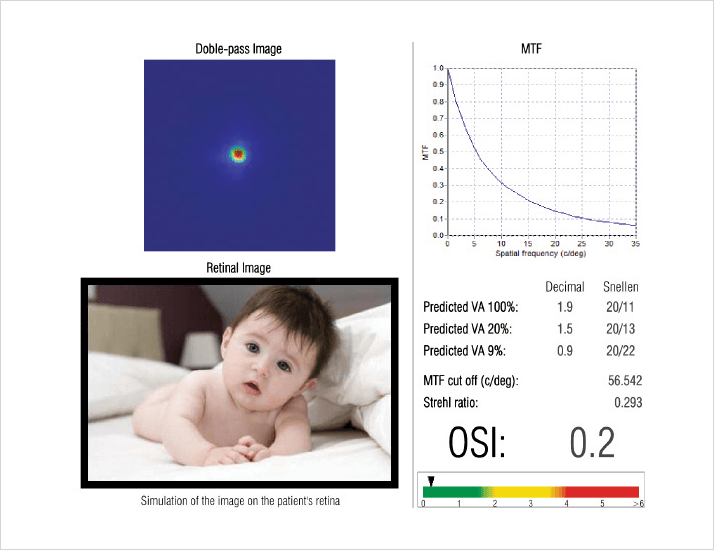
The importance of objective assessments of overall visual quality is increasingly appreciated. Health of the tear-film, ocular light scatter, clarity of the lens and depth of focus can all impact the results of LASIK, cataract and corneal inlay surgeries. Diagnostic devices, like the AcuTarget HD (AcuFocus, Inc.), optimize clinical outcomes within a cataract and refractive practice by offering a broader range of functionality and an objective assessment of overall vision. This instrument monitors tear-film quality over time, measures depth-of-focus, assesses pre- and postoperative inlay centration, and enhances patients’ understanding of the importance of postoperative care (see Figure 1).I have found the AcuTarget HD to be most beneficial in refining selection of refractive surgery candidates by evaluating the optical quality of the eye and measuring the Ocular Scattering Index (OSI) (see Figure 2). When those metrics are abnormal, surgeons should consider what truly is the best refractive surgery option for that patient. For example, an OSI above 1.5 means that ocular transparency is not perfect. This may be caused by an early-stage cataract that can hardly be seen on slit-lamp examination, and that patient may benefit from cataract surgery or clear lens extraction.
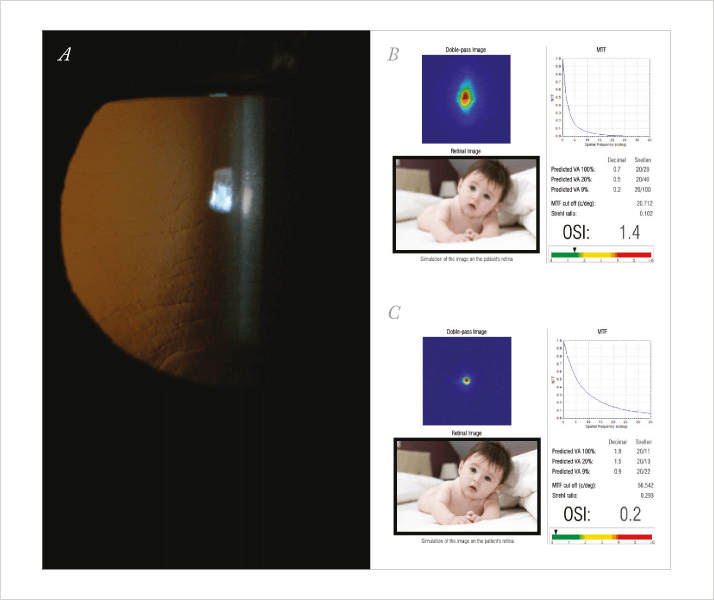
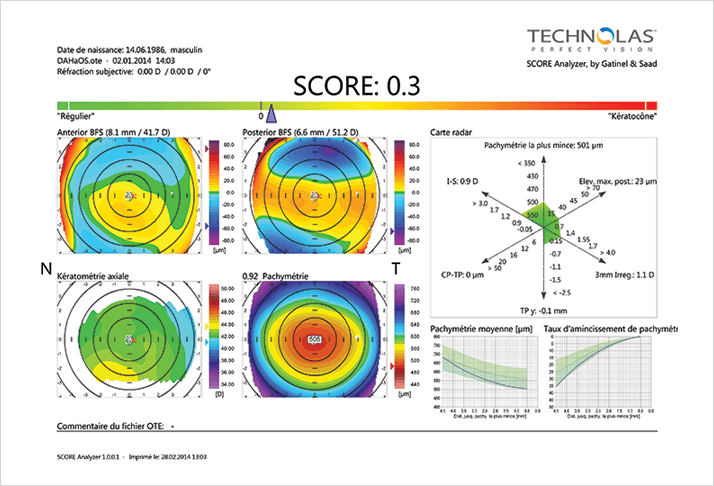
The AcuTarget HD also evaluates tear film and dry eye. This is of paramount importance to refractive surgeons for treating and eliminating dry eye pre-operatively, which tremendously improves outcomes. As a summary, the device provides a final image, which simulates both perfect vision and the patient’s vision, enabling the surgeon to compare the two images and gain a better understanding of what the patient is seeing. It helps explain patient symptoms and thus guides us toward the appropriate postoperative management. Topographers, such as the Orbscan (Bausch + Lomb), help refine refractive surgery outcomes by allowing us to detect abnormal topographies, which are a contraindication for refractive surgery. The Orbscan topographical maps can be screened by SCORE analyzer (Technolas Perfect Vision), a new artificial intelligence system allows the detection of subclinical keratoconus (KC) with a high sensitivity and specificity. I use it for every patient’s preoperative refractive and cataract surgery evaluation to detect abnormality in the cornea (see Figure 3).
An aberrometer (OPD-Scan, Nidek) is useful for patients in whom I plan to implant a toric or multifocal IOL. If the patient presents a large amount of high-order aberrations, preoperatively, he or she is considered poor candidate for a multifocal intraocular lens (IOL). The aberrometer also provides the exact amount of corneal astigmatism and the axis of the astigmatism, which allow correct toric IOL implantation. Although I don’t use the OCT (Visante, Carl Zeiss Meditec) for every patient group, it is useful in performing enhancements. When I am correcting myopia in a patient who has already undergone LASIK, OCT can determine the thickness of the old flap and the residual stromal bed, so I know the amount of tissue I can photoablate safely. Femtosecond lasers, like the iFS (Abbott Medical Optics), or the FS 200 (Alcon) have helped refine the surgical procedure by increasing the safety and the accuracy of flap incisions. Anterior and posterior stroma do not react in the same way to the femtosecond laser pulse, thus it’s important to have the data to enable you to program the laser settings for spot and line separation, energy level, and desired depth of the incision.
Clinical studies
Research has shown that the two leading causes of reduced optical quality after cataract and refractive surgery are uncorrected refractive abnormalities and increased media opacities that cause increased light diffusion (3). We evaluated the repeatability of measurements with a double-pass system (4). Forty-two eyes were separated into two control groups, a post-refractive surgery group and a cataract group. Measurements were taken using the HD Analyzer’s Optical Quality Analysis System (OQAS, Visiometrics), which measured the effect of high-degree optical aberrations and loss of transparency of ocular tissues on the quality of the retinal image. The main outcome measures were OSI, the cutoff frequency of the modulation transfer function (MTF), and the Strehl ratio. The repeatability limit for both groups was 0.841 (33.5%) for the OSI, 8.499 (31.1%) for the cutoff MTF, and 0.051 (31%) for the Strehl ratio. The repeatability limit was good and equivalent for the OSI, the MTF, and the Strehl ratio values, and there was a large gap between the normal and pathologic threshold for OSI measurements, indicating that the reliability of the double pass system complies with the requirements for quantitative assessment of scattering. We think that the double-pass system will play an important role in daily clinical practice in the near future. Diagnostic and surgical planning instruments not only restore vision, but also enhance it. As long as surgeons continue to screen patients appropriately, they will have continued success in refractive surgery outcomes. Alain Saad is an ophthalmologist in the Cornea, Cataract and Refractive Surgery Department (Damien Gatinel Department) at the Rothschild Foundation in Paris, France.References
- S.V. Kulkarni et al.,“Long-term visual and refractive outcomes following surface ablation techniques in a large population for myopia correction" , Invest. Ophthalmol. Vis. Sci., 54, 609–619 (2013). S.S. Simon et al., “Achieving target refraction after cataract surgery”, Ophthalmology, 121, 440–444 (2014). F. Díaz-Doutón et al., “Comparison of the retinal image quality with a Hartmann-Shack wavefront sensor and a double-pass instrument”, Invest. Ophthalmol. Vis. Sci., 47, 1710–1716, (2006). A. Saad, M. Saab, D. Gatinel, “Repeatability of measurements with a double-pass system”, J. Cataract Refract. Surg. 36, 28–33 (2010).
