
Abhay Vasavada: Ninja George, do you remember last year we had some problems – we taught somebody how to remove an IOL… and what happened? George Beiko: I do, Sensei. We taught David Chang, but he doesn’t remember! Abhay Vasavada: And that’s why we kicked him out of the dojo! George Beiko: This year I will show him how to take the lens out of a 3 mm incision rather than a 6 mm incision. I think that man can learn.
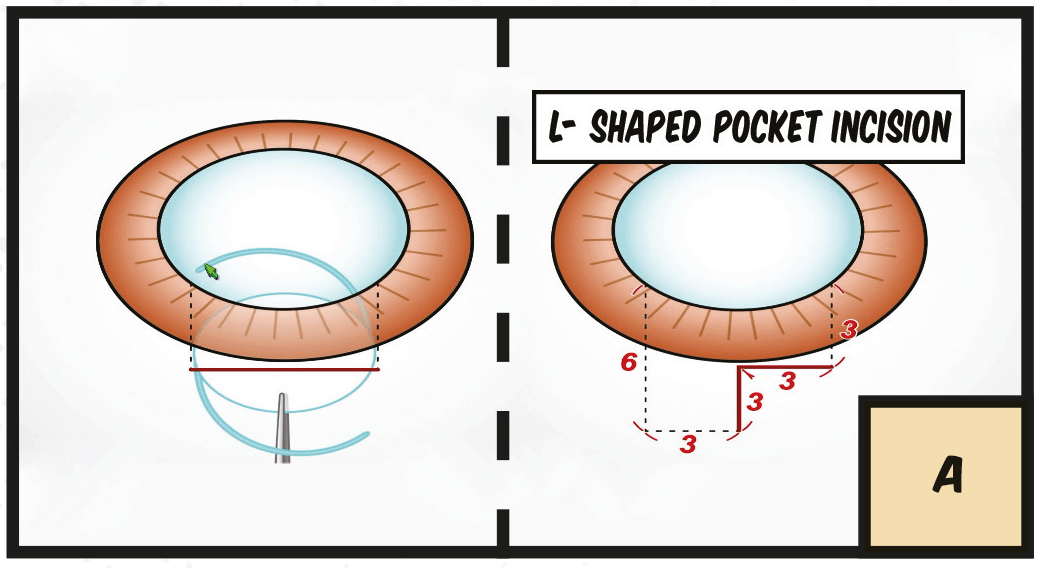
A. Typically, we put IOLs in through a 6 mm incision, but this means you risk inducing astigmatism and vitreous prolapse. Here’s the idea – first performed by Lawrence Brierley back in the nineties: a 3 mm incision at the limbus, going back 3 mm, and then tunneling through the sclera and the cornea in order to place the lens.
B. So, the technique can be used for putting in IOLs, or for taking out dislocated IOLs.
C. And I’ll show you first of all putting in an IOL, so the idea is 3 mm at the limbus, going back 3 mm, and then tunneling in order to get the other 6 mm.
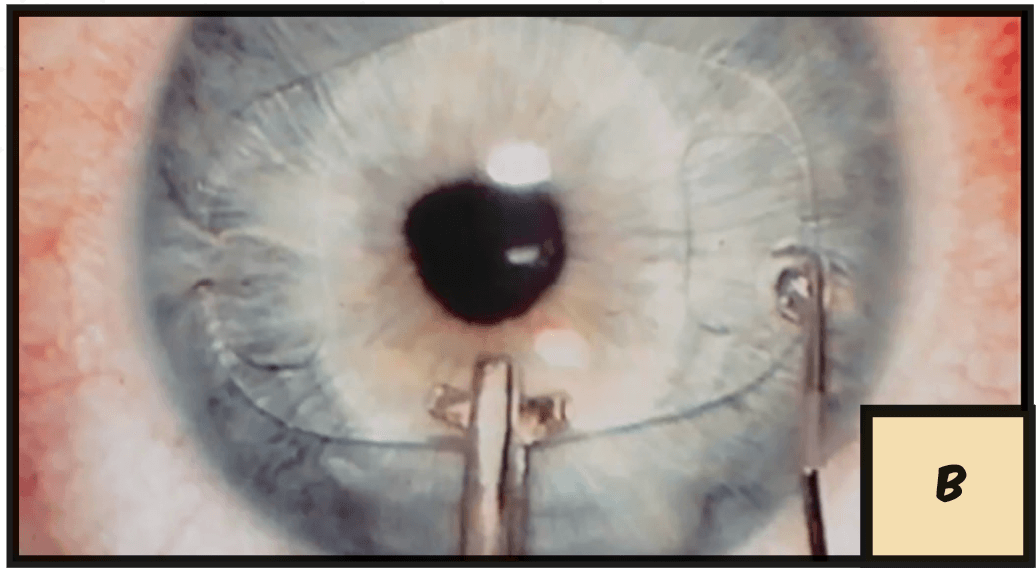
D. We mark it (the pupil is miotic because for IOLs you want that).
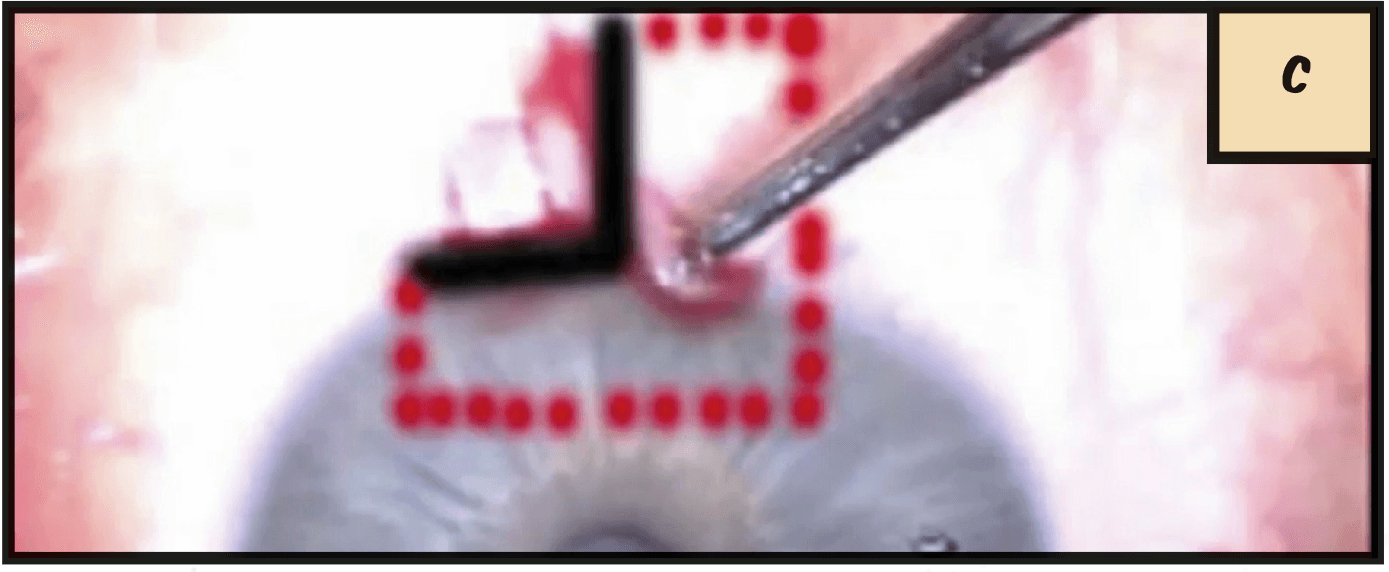
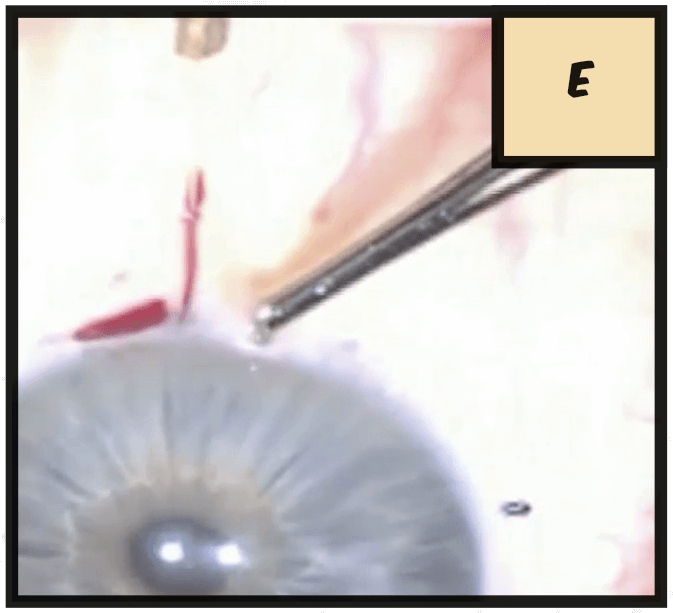
E. We make our groove, go back 3 mm, and at this point you can either use a blunt keratome or a diamond.
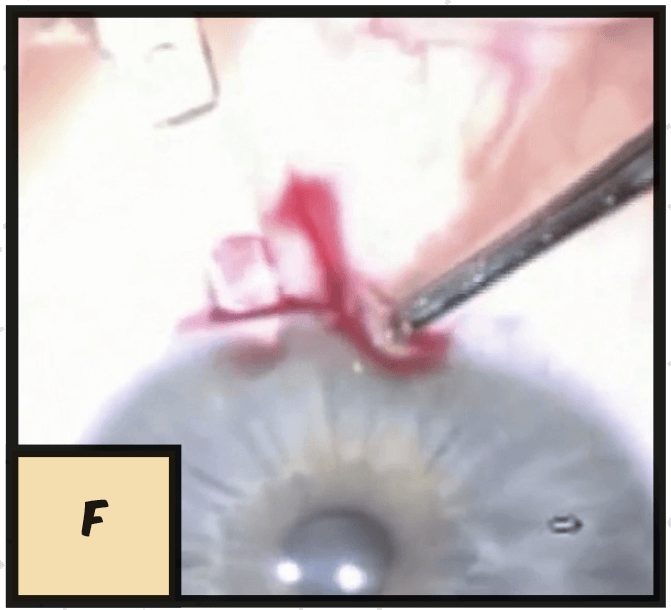
F. I felt comfortable enough with the procedure to continue on with the diamond. So we tunnel in, being careful not to penetrate the anterior chamber until we create the whole incision.
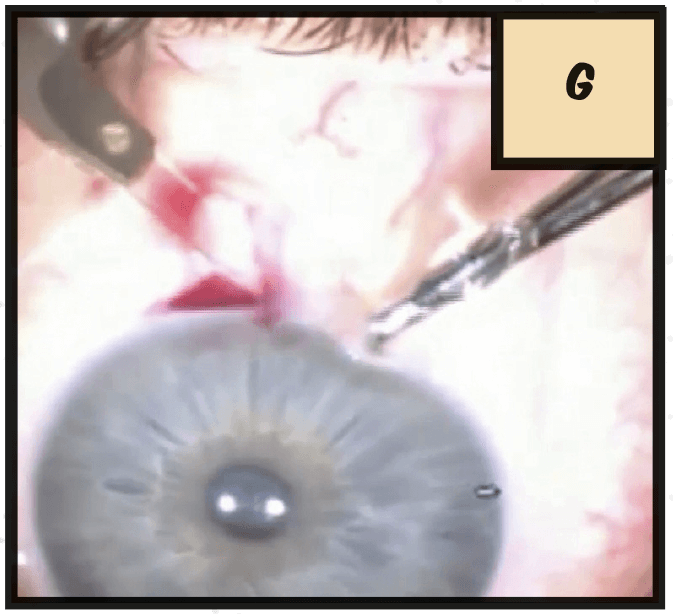
G. George Beiko: I wonder where David is, because we could show this to him again, seriously.
Abhay Vasavada: David, are you listening?
H. Put the viscoelastic in, so now you have your incision and the lens can fit through. You hydrate that wound, and I don’t use sutures. I like to use MST forceps in order to enclavate, so you can use this to put lenses in…
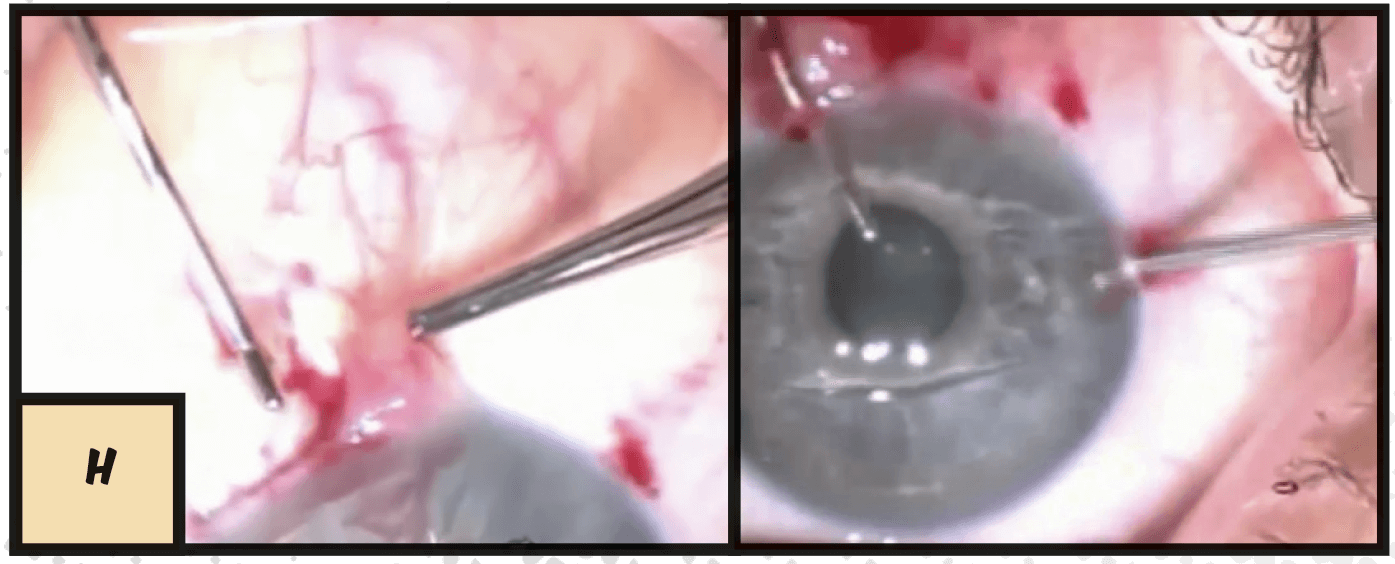
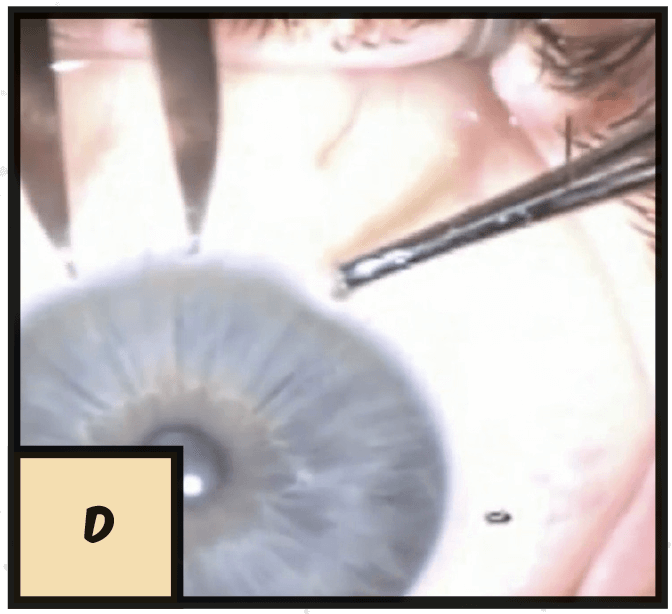
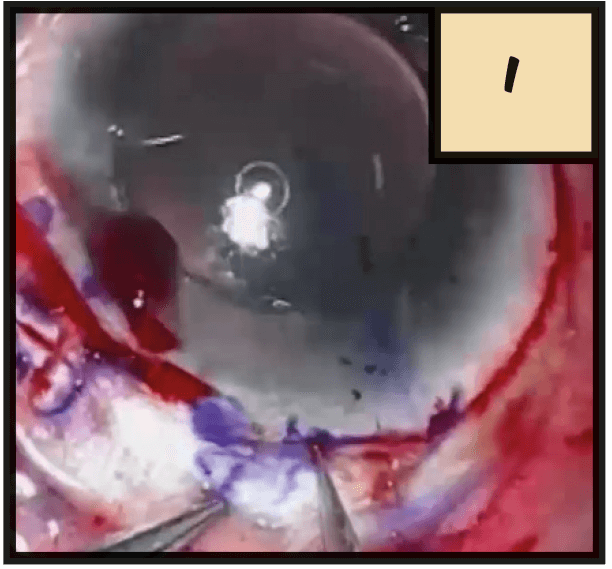
I. ... and you can also use it to take lenses out. In this case, the plan is to remove this PMMA lens and replace it with a lens that’s a more appropriate power for the eye. So I’m using a blunt dissection.
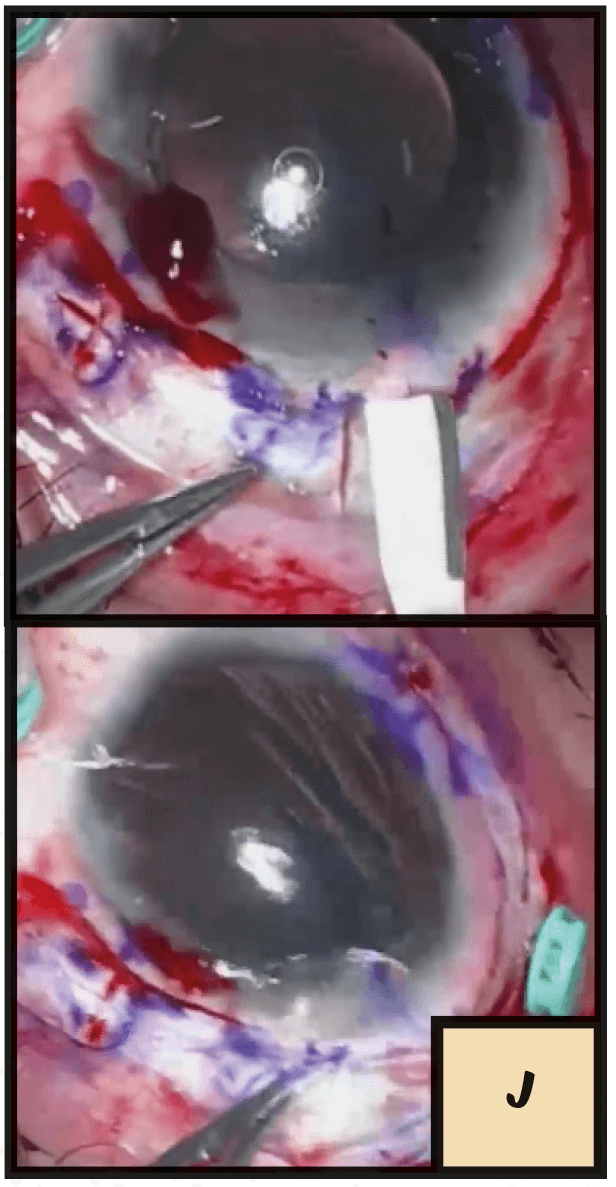
J. Again, 3 by 3, by 6, enter. The IOL easily comes out of the eye.
K. We place a 3 piece lens back into the eye, and externalize the haptics, and then you can either glue them or fixate them with the suture.
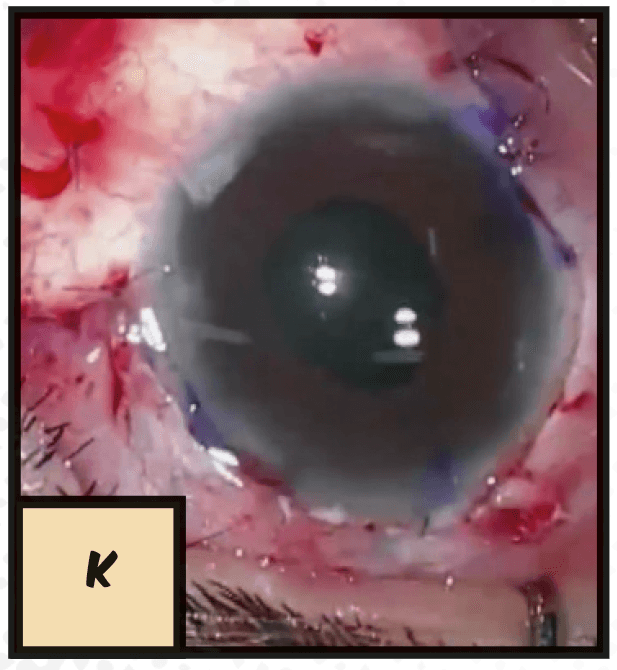
We performed keratoscopy immediately afterwards and 3 months later – and not one case showed a change in topography.
Ophthalmology on Ice Aye aye captain, ARRR! Captain Ectopia (Lentis)
