
If you are not nearsighted yourself, someone close to you will be: there is nothing more commonplace. Compensated for with a pair of spectacles or contact lenses it is, at worst, a mild inconvenience to most of us.
Why then is there a spreading unease across the world – culminating in near-panic in certain East Asian countries – over myopia? The answer is that this most homey of medical conditions is transforming rather quickly into an irascible monster. Its prevalence is through the ceiling. A recent survey in South Korea revealed the almost surreal fact that essentially all 19 year-old males there are myopic. Their military has compulsory conscription at that age, and 96.5% of conscripts are myopes. And it can be much more than a mild inconvenience. High myopia, usually defined as a spherical equivalent >6.00 diopters, is said to affect around 2 percent of the population in the United States and Europe – and 21.6 percent of those Korean conscripts. High myopia is a major cause of legal blindness due to increased risk for premature cataracts, glaucoma, retinal detachment and macular degeneration. As Ian Flitcroft of the Mater Hospital in Dublin, Ireland puts it, “Three diopters of myopia is worse for your eyes than 20 cigarettes a day is for your heart.”
Now, the scary part. We have no clear understanding of the mechanism by which myopia develops, which means we can do absolutely nothing to prevent it from occurring, and once it starts we have precious little idea about how to contain it. This article poses five questions concerning the myopian dystopia that is enveloping us and looks at science and medicine’s present day best answers. The questions are:
- What are the current and likely future impacts of myopia on health and the economy?
- What are the mechanism by which myopia develops?
- What factors contribute to susceptibility to myopia, and how do they do so?
- What are the current and potential treatments for myopia?
- How do we move towards prevention of myopia?
How thoroughly we can answer these questions, and how quickly we can implement potential solutions, will determine the impact that myopia will have on the current and future generations. The one certain thing right now is that this is not your father’s near-sightedness.
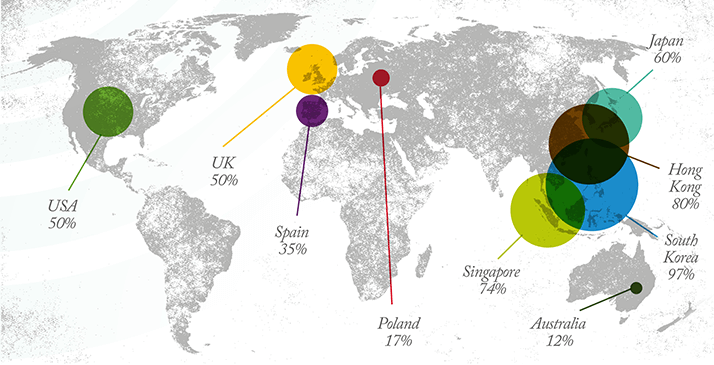
Question 1. What are the current and likely future impacts of myopia on health and the economy? The reach of myopia is well illustrated in adolescents (Figure 1). Following well-documented increases in prevalence over the last three to four decades, currently 25 to 50 percent of adolescents in the West and between 60 and 100 percent in East Asia are myopic. The burden extends well beyond the period of transition to adulthood, of course, and back-of-the-envelope calculations suggest that there are 200 million myopes in the world today; by 2020, there may be 900 million. The prevalence in young adults results from a gradual increase in cases per year throughout childhood. Myopia often becomes apparent in school-age children, although the problem may have its roots even earlier in life. Indeed, the prevalence of myopia in Singapore Chinese children aged 6 to 72 months stands at 11 percent. Rates vary dramatically with ethnicity and with location, providing clues to the genetic and environmental factors that underlie the epidemic. Chinese children are more likely to be myopic than any other ethnic group, while the prevalence in Asian children generally is higher than in European children. There is also a distinct division between urban and rural areas. Population studies of paired groups with similar genetic backgrounds in India, Nepal and China, for example, consistently demonstrate a lower prevalence of myopia in children from rural locations.
The most serious concern is the rising numbers of patients with high myopia. This is a feature across the world but is most pronounced in East Asia, where a number of studies have reported prevalence exceeding 20 percent; in the West, the figure is in the low single digits. High myopia especially involves the macula. Potential complications include choroidal neovascularization, myopic chorioretinal atrophy, myopic macular retinoschisis, myopic macular holes, lacquer cracks and posterior staphyloma. The optic nerve may also be affected, causing myopic conus and myopic optic neuropathy. And a final problem is that the results of refractive surgery are less predictable. This alarming menu illustrates the need for concerted action on the part of public health organizations everywhere. In looking at the economic impact, the spotlight must first be shone on developing countries. “Avoidable distance vision impairment,” caused by problems that are readily addressed with spectacles and contact lenses in other parts of the world, has been estimated to cost $202 billion per annum by The International Agency for the Prevention of Blindness (IAPB). But the economic cost is dwarfed by the humanitarian toll of uncorrected refractive errors. The problem could be eliminated, according to IAPB, by an investment of $28 billion to establish the required eye care services. To promote this solution, IAPB proposes to integrate eye care into the United Nation’s post-2015 Millennium Development Goals. It is a logical fit, given that the Millennium Goals are geared to improving economic, social and health outcomes. How about the developed world? A survey in the United States estimated that in 1990 the price of correcting vision impairment owing to refractive error was between $3.9 billion and $7.2 billion. This figure was based on the direct costs of providing spectacles to everyone over the age of 12 who need refractive correction to achieve good distance vision. While this is a big number, it is dwarfed by the heavyweights of healthcare, the chronic diseases: for example, spending on dementias including Alzheimer’s disease topped $200 billion in 2012, while diabetes cost $245 billion and heart disease and stroke combined accounted for $312 billion. Given a doubling in the number of myopes since the study was published, plus the fact that no costs beyond the provision of eyeglasses were included, it is not hard to imagine that the annual cost to the US of refractive errors runs to several tens of billions. (As a whole, eye and vision disorders cost about $140 billion in 2012). And these costs will continue to climb steeply if solutions are not forthcoming.
Question 2. What is the mechanism by which myopia develops? Despite a century of interest in refractive development, the etiology of myopia is still not fully understood. Now, with the prevalence skyrocketing, the search for answers is more urgent than ever. What is known is that myopia results when an eye is too long for its optical power or optically too powerful for its axial length. The components of the optical system, such as axial length, refracting power of the cornea and depth of the anterior chamber, must remain in sync as the eye grows to ensure that objects are brought into sharp focus. The hypothesized mechanism by which this is brought about is called emmetropization, a term derived from the Greek emmetros, meaning “well-proportioned” or “fitting”. Identifying aspects of the visual experience that might aid, or hinder, the process of emmetropization provides clues as to why myopia develops. Several factors have been identified; the mechanism du jour is that outdoor light exposure helps maintain emmetropia. Spending too much time indoors, and not enough time outdoors promotes myopia. There are a couple of mechanistic explanations for this indoor/outdoor light phenomenon. These explanations are not mutually exclusive. One is the huge disparity in the level of light exposure. Outside, light level readings are in the range of 50-100,000 lux; indoors, values are less than 1,000 lux, and mostly closer to 500. Increased exposure to sunlight promotes dopamine neurotransmission in the retina; in animal models, dopamine signaling is associated with an inhibition of axial elongation. Thus, a child exposed to a sufficiency of outdoor light is less likely to develop myopia than if he or she spends most of the time indoors.
Another possible mechanism involves peripheral vision. An outdoor vista, such as that experienced at the ocean or in the countryside provides dioptric continuity throughout the visual field: both central and peripheral vision are clear, unblurred. This state may help maintain symmetry of the eyeball, and promote emmetropia. Indoors, dioptric stimuli vary widely across the visual field. Central vision may be focused on a television screen or words on a page, but a wide range of light sources and objects at different distances means that the peripheral retina is likely to be defocused. Studies in animal models indicate that this kind of optically-imposed defocus impacts upon central refractive development: when the periphery of the eye is defocused, refractive errors are more likely to occur. Hence, the child spending his or her time indoors is more inclined to be myopic. Increased understanding of the factors that influence refractive parameters and how these interact should lead to more effective treatments to slow myopia progression or to prevent its onset.
Question 3. What factors contribute to susceptibility to myopia? Nature or nurture? There is clearly a mix of genetic and environmental components involved in the development of myopia, but the contribution of each, and the ingredients that make up that contribution, are still being teased out. Back in 2005, a meta-analysis of some 300 papers downplayed the role of hereditary factors. It noted distinct variations in prevalence between genetically similar cohorts in different environments: for instance, the high prevalence of myopic Indians in Singapore (70 percent of 18-year-old men), while in India itself the rate was roughly 10 percent. The simplest explanation of such findings is that a massive environmental effect is swamping the genetic influence. So, was mother right when she said, “Don’t stare at the television too long or your eyes will go square”? No. Despite the folklore of “screens damaging eyes,” which has been passed down the generations in the form of watching TV, playing video games, working with personal computers, to today’s use of smartphones, their impact appears to be minimal. What Mother failed to identify is the crystal-clear relationship between education (and socio-economic status) and myopia prevalence in children. “Education” likely means “more reading,” supporting the idea that “nearwork” is a significant risk factor in myopia. Additionally or alternatively, increased indoor activity means less outdoor activity. As noted above, a strong body of evidence links outdoor activities, such as sports (though not indoor sports) and the amount/duration of sunlight exposure, to reduced risk of myopia in children. Thus, for “environmental factors,” read “lifestyle”; an important distinction when comparing myopia incidence on a global scale.
Environmental factors alone cannot, however, explain why so many individuals within a single family present with myopia; there must be a substantial role for genes. Altogether, an extraordinary 68 genes across all chromosomes have been associated with refractive error, including 20-some recent additions from the international Consortium for Refraction and Myopia (CREAM) and the company 23andMe, who corroborated each other’s findings. Interestingly, no significant genetic differences between Europeans and Asians were discovered. The bad news is that many of the genes have very slight (though additive) effects, ruling out a simple solution. The rather better news is that they can be mapped onto functional pathways, giving pointers on how to improve our basic understanding and, by extension, our ability to treat this perplexing condition. The pathways include neurotransmission, vitamin A (retinol) metabolism, eye development and remodeling of the extracellular matrix. Rapid progress is being made on the environmental component too. Randomized clinical trials are underway to more precisely pin down the impact of sunlight, bright light, and/or outdoor exposure; some of these studies use wearable light sensors in place of questionnaires to capture data more rigorously. The ultimate goal will be to integrate the two streams of information, pinpointing unfavorable combinations of genetic predisposition and environmental factors that are particularly risky for the development of myopia. At that point, improved therapeutic options may come into focus.
Question 4. What are the current and potential treatments for myopia?
Spectacles, contact lenses and intraocular lenses bring the image closer to the retina, helping to render a sharp, focused image. For patients with low, non-progressing myopia (-3.00 diopters or less), that’s great. But for those with mid or high myopia, and especially for children with progressing myopia, strategies that reduce the rate of progression are highly desirable.
Here’s a selection of effective approaches:
Behavioral interventions
A meta-analysis of studies that looked at the effect of increased outdoor time on children’s risk of myopia (2) concluded that each additional hour spent outside per week reduces the odds of myopia by two percent. There are several potential (and non-exclusive) explanations for this, including the aforementioned increased exposure to sunlight. For example, pupils are more constricted outdoors than indoors, which increases the depth of focus and reduces blur, slowing eye growth. Another theory points to an assumed reduction in nearwork given that more time is spent outdoors, while a further suggestions is that physical activity itself prevents myopia.
Pharmacological interventions
Pharmacotherapy with muscarinic receptor antagonists like atropine and pirenzepine has been evaluated, initially because accommodation appears to play a role in the progression of myopia.
The use of 1% atropine is effective in slowing childhood myopia progression. However, the decision to administer drugs to children over an extended period must always be approached with care. Atropine’s side effects include blurred vision, increased light sensitivity and constantly dilated pupils, making it commercially impractical. More recently, 0.01% atropine has been evaluated; it also slows the development of myopia, but with less cycloplegia and better tolerability. A further bonus is that there are lower levels of rebound progression on the termination of treatment. Pirenzepine has also been evaluated in a randomized placebo-controlled trial: relative to placebo, a 2% gel formulation administered twice-daily almost halved the rate of myopia progression in children.
Optical interventions
Orthokeratology – or overnight vision correction – uses specially designed rigid gas-permeable contact lenses that reshape the cornea, reducing the extent of myopia and correcting vision in the short-term for adults. In children, there is an additional benefit: the rate at which the eye’s axial length elongates is reduced, slowing the development of myopia. A recent study showed that progression of myopia in children wearing orthokeratology contacts was significantly less than a control group over a two-year evaluation. Orthokeratology is said to be effective up to -4.00 diopters.
Bifocal soft contact lenses (BSCLs) with a distance center may provide a similar effect as corneal reshaping. One comparison of BSCLs against single-vision soft contact lenses (SVSCLs) in children showed significant slowing of both myopic and axial length progression. Soft multifocal lenses appear to have similar effects in children; in a recent clinical trial, the rate of myopia progression was halved, and axial elongation reduce by one third compared with SVSCLs.
Surgical interventions
For adults (though not for children save in a small number of special cases) there are several surgical techniques that can be employed. They have no effect on the underlying posterior segment pathology: existing axial eye elongations are not reversed, the vitreous chamber continues to lengthen unabated, and the risk of posterior segment sequelae remains.
Laser procedures have been used to treat nearsightedness in around 50 million adults over the past 20 years. The cornea is reshaped by removing a small amount of eye tissue using a highly focused laser beam. Recent developments include the cutting and extraction of a lenticule, a disc-shaped piece of corneal tissue.
Phakic intraocular lenses (IOLs) are gaining currency for moderate and high myopes. The implanted lenses have the advantage of being removable, and their effects reversible.
Question 5. How do we move towards prevention of myopia? Since axial lengthening of the eye isn’t reversible, the only way to prevent myopia is to stop it developing in the first place. That means intervention in children, as soon as signs of near-sightedness appear – which could be in infanthood. At present, no single strategy can prevent childhood myopia. However, shrewd combinations of current tactics, based on novel clinical algorithms and public health initiatives, are having a marked impact. Perhaps the best example is from the Singapore Health Promotion Board which for many years has rigorously assessed vision in schoolchildren and spent millions of dollars on national myopia prevention programs to educate the public. Regular screening of children’s vision – something that’s already practiced in many urbanized parts of the world (where the issue is most acute) – is an essential part of any strategy. This must include not only school visits by optometrists but assessment of younger, pre-school children and even babies. Myopia develops most rapidly in the initial couple of years – and it’s during this period that interventions can make the biggest difference. The emergence of Myopia Control Clinics, such as the one at the University of California Berkeley (www.caleyecare.org/myopia-control-clinic), will help ensure efficient delivery of treatment to myopic children and young adults. “In addition to providing conventional glasses to correct myopia,” their website explains, “doctors will be offering treatments for controlling the condition’s progression, ranging from special contact lenses to prescription eye drops.”
Refractive interventions in children – from orthokeratology to soft bifocal contact lenses – certainly have a place in a myopia control strategy. Such approaches work for many children, but the extent to which they prevent myopia progression is unpredictable. It’s an area that is continually evolving, and more effective contact lenses are likely to be introduced periodically. Other components of a fully integrated strategy are more easily stated than implemented. For example, having children spend more than two hours a day outdoors does seem to prevent – or at least substantially retard – the development of myopia. However, today, the average American kid spends under 30 minutes a week in unstructured outdoor play, while devoting seven hours indoors in front of electronic screens. In other countries, parental obsession with academic attainment is an equally large obstacle to outdoor play. It is going to take a concerted and creative marketing campaign to nudge families into changing their lifestyles. Again, Singapore offers an example of one way forward. The program there was initiated around 15 years ago, built around the message to take breaks from nearwork. Since the importance of outdoor exposure became known, some eight years ago, programs directed at parents, schools and schoolchildren themselves have made outdoor activities an essential part of the day. In the past five years, the rates of myopia have almost stabilized, contrasting dramatically with the rapid growth in the previous three decades. Notably lacking from most current myopia prevention strategies are pharmaceutical interventions. While atropine and pirenzepine are effective, their anticholinergic side effects have precluded prescription (though hopes for 0.01% atropine remain high). The search for new agents that have a better therapeutic index with fewer side effects is underway and may benefit from the growing body of genetic information. Who would bet against such remedies being found? The size of the market provides great incentive to industry. The “database state,” where healthcare, governmental and commercial records are all maintained electronically, means that almost population-wide assessments of public health and the impacts of interventions can be made rapidly, and far more easily than what was previously the case. The highly myopic eye is a vulnerable eye. Reversing the prevalence of myopia – across the entire globe but especially in East Asia – presents a monumental social, scientific, medical and political challenge. The lack of a “magic bullet” and of a sophisticated knowledge of the mechanism by which myopia develops complicates matters. But the stakes are high. There is a real prospect of everyone being nearsighted in certain locations, including huge numbers of high myopes who will have significant vision-related problems. A solution seems to be emerging but it will require great discipline and deep pockets to implement. Hopefully, innovations will continue to bring that solution within more certain reach.
References
- I Morgan and K Rose, “How genetic is school myopia?”, Progress in Retinal and Eye Research, 24, 1–38 (2005). JS Sherwin, MH Reacher, RH Keogh, et al., “The Association between Time Spent Outdoors and Myopia in Children and Adolescents. A Systematic Review and Meta-analysis”, Ophthalmology 119, 2141–2151 (2012)
