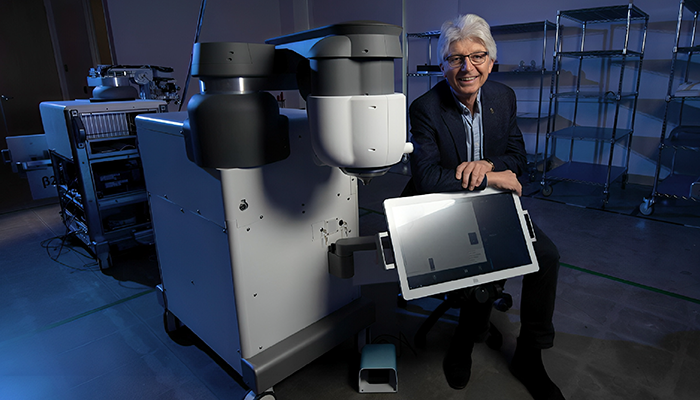
Headshot supplied by Tibor Juhasz
Having obtained a PhD in physics, what drew you to ophthalmology?
It really started by accident. After completing my PhD in Hungary, I was lucky enough to be offered a research position at the University of Rochester, New York, with Gérard Mourou – the world leader in ultrashort pulse laser technology at the time. (Important sidenote: for this work, Mourou and Donna Strickland would go on to be awarded the 2018 Nobel Prize in Physics). After a short time in Rochester, I spent several years in Southern California, doing postdoctoral research and continuing to work in laser technology, including consulting for a company that was evaluating laser applications in ophthalmology. That effort was unsuccessful because we needed much shorter laser pulses to achieve the desired effects.
Eventually I rejoined Mourou in his new lab at the University of Michigan, where he was focusing solely on femtosecond lasers. One day, one of Mourou’s graduate students inadvertently lifted his safety goggles and caught a stray laser beam, causing a retinal injury. The student was sent to one of the university’s ophthalmology residents, Ron Kurtz, who checked out the injury and got very excited to find that the damage to the retina was extremely small and confined, without any collateral damage. Suddenly, we were all much more excited about ophthalmic applications for femtosecond lasers! Our work together demonstrating the femtosecond laser’s capacity to create ocular tissue incisions with micron-level precision without damaging adjacent tissue would ultimately revolutionize laser refractive surgery, cataract surgery, and corneal transplantation.
What were the challenges of bringing femtosecond laser technology to the world's attention?
One problem was that the lasers were very big – filling an entire lab! Plus, you needed at least a couple of graduate students to run around them all day making adjustments to keep them operating. So, the first challenge was to engineer a femtosecond laser that could sit in a small, confined area. The second challenge was to make the laser more stable and less expensive to operate.
Although we recognized that there were many potential applications for the femtosecond laser in ophthalmology, we began with flap creation for refractive surgery. At the time, lamellar flaps were made with a microkeratome, but it was difficult to achieve a consistent thickness and the bladed flaps were prone to complications. The femtosecond laser significantly reduced both the uncertainty and the complications, making LASIK safer and more predictable for patients.
When did you realize that the femtosecond laser would become a widely used tool in ophthalmology?
Ron Kurtz and I founded the company IntraLase as a spin-out from the University of Michigan in 1997. Though we were convinced femtosecond lasers would work, doing so in a cost-effective way remained a challenge. It wasn’t until the early 2000s that we were able to introduce the technology to the marketplace and see it begin to take off. Steven Schallhorn, the lead ophthalmologist for the Navy in San Diego, began using the laser in practice and found the femtosecond laser-created lamellar flaps to be very stable, with excellent clinical results. The data he gathered and presented at conferences affirmed the technology and convinced other clinicians it was a worthwhile investment. After that, we saw a rather rapid uptake of femtosecond laser technology in corneal refractive surgery. Bladeless, femtosecond laser LASIK has for years been considered the standard in the field, and more than 24 million patients have benefited from it.
What are you currently focused on in the laser space?
Today, I am focused on glaucoma because I feel there is a real unmet medical need in this area. There are many treatment options for glaucoma patients, but they all have shortcomings of some kind. The femtosecond laser can be used to create drainage channels through the trabecular meshwork. The channels increase the outflow of aqueous humor, thereby decreasing intraocular pressure (IOP) without damage to the adjacent tissues. And, because the femtosecond laser beam can be delivered through the cornea, the procedure can be performed completely non-invasively, without opening the eye. This minimizes or eliminates surgical trauma, speeding up recovery.
How does this process improve on current micro-invasive glaucoma surgery (MIGS)?
MIGS is similar in that it creates an opening in the trabecular meshwork (TM), but in most cases it also involves implantation of a stenting device into the TM. It can be hard to visualize and correctly place the stent and, of course, the patient has undergone corneal incisions to achieve this goal. With an incision-free, precise, femtosecond approach, creating the TM opening can be done noninvasively in a way that is more reproducible and easier to visualize, thereby making it more accessible to a wider range of ophthalmologists and their patients.
How far away are we from seeing femtosecond lasers in glaucoma surgery?
We’re now three years out from a pilot study to evaluate the safety and efficacy of the procedure we call FligHT (femtosecond laser, image-guided, high-precision trabeculotomy) (1). In the cohort studied we have seen no serious adverse events and a mean IOP reduction of approximately 34 percent at the two-year timepoint. I think the study indicates that FLigHT is going to be a potentially safe and effective procedure. For example, it creates a single channel – measuring only 500-μm wide by 200-μm high – through the TM and into Schlemm’s canal. I can see this working very well as a first-line treatment; it can also be used in patients who are either phakic or pseudophakic who are unhappy or uncontrolled on IOP-lowering medical therapy.
What stands out for you as a particularly proud moment in your career?
As R&D team leader at IntraLase, I was delighted to put the very first femtosecond laser into the market, when everyone told me it was impossible and when even the laser experts told me the technology was just too complex and too expensive to be engineered for use in ophthalmology. I’m proud that we succeeded and that we now see femtosecond lasers being widely used in clinical practice for refractive, cataract, and corneal surgical applications. The safety and efficacy of FLigHT appears to be favorable based on our first-in-human study, so I believe we will defy the odds again by successfully bringing to market the first device capable of performing a noninvasive, non-incisional trabecular bypass procedure in glaucoma.
References
- ZZ Nagy et al., “First-in-Human Safety Study of Femtosecond Laser Image-Guided Trabeculotomy for Glaucoma Treatment: 24-month Outcomes,” Ophthalmol Sci., 3, 100313 (2023). PMID: 37363134.
