How well are you communicating with your patients? A recent study by researchers from the University of Michigan Kellogg Eye Center found significant differences between self-reported eye symptoms experienced by patients and the entries on their electronic medical records (EMRs). To discover the extent of the disparity, the team carried out an observational study, in which patients filled out an eye symptom questionnaire before their appointment with an ophthalmologist.
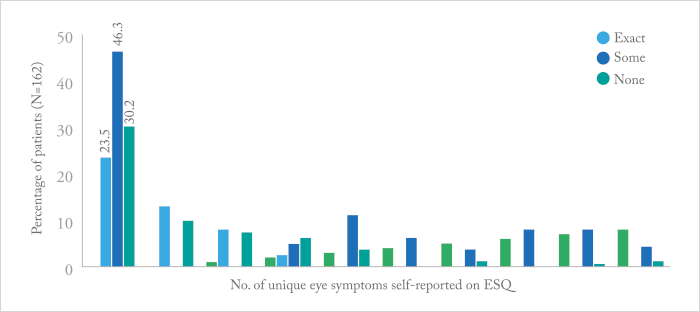
The investigators compared the presence or absence of blurry vision, glare, pain/discomfort, redness, burning/stinging, itching, gritty sensation, and sensitivity to light. And of the 162 patients studied, only 38 (23.5 percent) had an “exact agreement” between their medical records and the pre-appointment questionnaire (Figure 1).
And though it might seem like a worrying statistic, it isn’t necessarily surprising, according to Paula Anne Newman-Casey, co-author of the associated paper (1). “Issues with doctor-patient communication are age-old and some issues will continue regardless of whether notes are taken on paper or electronically. In the era of paper charts, the purpose of a medical record was to allow the physician to document the history of the illness and diagnosis plan for each patient, not to be a compendium of information to facilitate the measurement of the quality of care delivered,” says Newman-Casey. “Any unrecorded symptoms are not necessarily missed ones – when speaking to their doctor, patients may focus on some symptoms more if a particular thing is bothering them. But because EMRs allow researchers and others to extract information in a way that has never been previously possible, the implications of capturing patient data in the most accurate way becomes much more imperative.” Newman-Casey suggests that pre-appointment questionnaires could actually be the way forward – patients could offer information on their symptoms on a tablet in the waiting room, which could be monitored over time to see what effect any treatment was having. The information could also be used on a wider scale to improve healthcare overall by better capturing both symptoms and patient-centered outcome measures. “The data captured in the electronic health record, if it is highly accurate, can be used to improve the quality of care that we deliver in a way that data captured on disparate paper charts never made possible,” adds Newman-Casey.
References
- NG Valikodath et al., “Agreement of ocular symptom reporting between patient-reported outcomes and medical records”, JAMA Ophthalmol, [Epub ahead of print] (2017). PMID: 28125754.
