- Sean Ianchulev’s company, Eyenovia, is using piezo-printing technology to change the eye-drop delivery process
- The new piezo-electric delivery system is capable of delivering small doses of 6-8 microlitres – volumes compatible with natural physiology
- The microdosing system will reduce side effects associated with the eye drop toxicity
Patients dislike glaucoma eye drops; the delivery mode is inconvenient and imprecise – in fact, unlike no other medical field, in ophthalmology we deliver the wrong dose more often than we do the prescribed one – with many studies now demonstrating that only one third to a half of all patients are able to successfully deliver the indicated topical dose to their eye (1). Most of the time they miss the eye altogether or deliver 200-500 percent overdose causing side effects, waste and missed compliance. Ophthalmic formulations cause a range of unwanted side effects from discoloration to periorbital dermatitis. Hence the famously high non-adherence levels associated with topically-applied glaucoma medication. But given that the standard eye-dropper method dates from before the 20th century, should we really be surprised that it’s problematic? Ianchulev certainly takes this view, and is indignant that the subject isn’t more broadly discussed. “Physicians are using a 150-year-old device to deliver 50 microlitres of drug into a seven microlitre tear film volume – no wonder eye drops are poorly tolerated!” But now Ianchulev’s company, Eyenovia, is bringing 21st century engineering to ocular drug delivery. “By marrying piezo-printing technology with smart drug delivery, we’re completely disrupting the eye-drop technology,” he says. In fact, the implications of the Eyenovia technology go far beyond issues of drug tolerability: some of the off-target effects associated with eye drops are life-threatening, and include cardiotoxicity symptoms, such as arrhythmia and bradycardia. So, by reducing off-target tissue exposure, Ianchulev’s microdosing approach may improve not just patient comfort, but patient safety – good news for patients, physicians and healthcare systems alike.
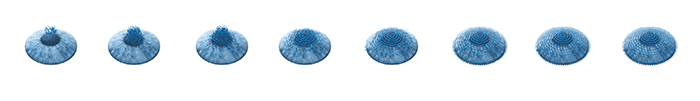
What’s new about the Eyenovia approach? Discarding the ancient eyedropper, Ianchulev’s team has turned to piezo-electric ink delivery systems – well known for precise delivery of suitable amounts of ink onto paper – by modifying such technology to administer 6–8 µL drug doses that are more compatible with natural physiology; in other words, the volume delivered does not overload the eye with fluid in the same way as an eyedropper. Louis Pasquale, Ianchulev’s clinical collaborator, makes another important point: “Keeping the administration volume to 8 µL or less is important; larger quantities cause a lachrymal reflex that washes much of the dose out of the eye,” he says. “When you think about it, it’s amazing that glaucoma eye drops work at all – much of the administrated dose is washed out by the lachrymal reflex.” Avoiding this wash-out is not only more efficient in terms of drug use, but also more pleasant for the patient.
We spoke to Louis Pasquale, a glaucoma specialist at Mount Sinai who is working with Eyenovia on the chronic angle closure glaucoma (CACG) trial.
Until recently, I was at the Massachusetts Eye and Ear Infirmary; now that I’ve moved to Mount Sinai, it’s easier to be actively involved in the Eyenovia CACG-latanoprost microdose trial. The Eyenovia collaboration has grown from work that Sean and I did on telemedicine and microdosing a few years ago. At that time, we were investigating the efficacy of microdosed phenylephrine for mydriasis. As an eye drop, phenylephrine can cause problematic side effects, not least elevated blood pressure. However, we showed that the microdose formulation has no such effect (1).
Now, we are following up the phenylephrine work with an investigation of microdosed latanoprost for CACG; current efforts are aimed at extending our recent proof-of-principle study on latanoprost microdosing. In the present trial, we have tested the product in 30 healthy volunteers, and demonstrated that latanoprost microdosing mediates IOP reduction equivalent to latanoprost eye drops at 80 percent lower total dose exposure, at least in the short term. And now that we have shown short-term efficacy, I’m helping to design a bigger trial, hopefully a six-month study. This will, inter alia, answer questions about topical and ocular side effects, which of course we would expect to be much lower for the microdose product than for eye drop latanoprost. The plan is for a large multi-center trial in 2019; New York might be one of the centers, because it has a huge volume of CACG patients and a wonderful clinical research centre. Overall, the aim is to have an FDA-approved device in patients’ hands within two years.
We also intend to look at the feasibility of self-administration by patients. That’s what the device is designed for: glaucoma is a chronic 24/7 disease, and ultimately we need a device that patients can operate themselves, so that they can manage their glaucoma independently. We’ll have to teach patients how to work the device, but we don’t anticipate many problems – it’s very straightforward. The device has an LED light; the patient looks at the light, and actuates the device; one spray, and eight microlitres of drug get printed onto the cornea. It couldn’t be simpler. And since the spray speed is faster than the patient’s blink speed, it will be very difficult to get that step wrong.
Looking ahead, this trial will hopefully kill two birds with one stone: it will give US physicians an effective product for CACG, and at the same time it will get the microdose device into the mainstream of glaucoma treatment. This is important – there is a real need for a product that significantly helps CACG management, and my view is that the time has come for us to consider alternative methods of drug delivery in this field. Eyenovia technology should also be a game-changer in the pediatric setting: dilating children’s eyes can be a little traumatic, and our system should be a better way of doing it. And there are many other opportunities for our system: for example, future products might include newly approved drugs and fixed combinations of older drugs. Microdosed atropine for slowing myopic progression in children is also very promising.
I have worked with Sean for some years now, and I’m very fortunate that he keeps involving me in his innovative ideas. The Eyenovia approach is a particularly exciting step forward, and I believe it represents a fundamental paradigm shift in terms of treating glaucoma patients. It is a long-overdue advance: even when I was a resident, back in 1987, I knew that the eye-dropper approach was problematic. When used correctly, they work, but we can do better. So that’s what the Eyenovia approach is about, and it’s great to be involved.
When and where
But it’s not just about how much drug is delivered. Piezo-electric technology is also precise (imagine if your inkjet printer was not!). Eyenovia’s device aims to accurately and uniformly coat the small volume of drug onto the corneal surface (where intraocular drug penetration occurs) (2). Could such efficient drug delivery also lead to less frequent administration? Time will tell.
In any case, microdosing intuitively indicates less drug-associated toxicity. And if the side effects are reduced, patients should hopefully be less reluctant to adhere to treatment regimens; hence, one of the first indications being explored by Eyenovia is glaucoma medication (Box 1), where satisfactory regime compliance is a long way off. In this context, it’s interesting that Eyenovia has taken compliance one step further by coupling an app that reminds patients when their dose should be taken with Bluetooth-enabled monitoring of device actuation. According to the Eyenovia website, its “intelligent electronic system is one of the first smart technologies to enter FDA clinical trials for ophthalmic use.”
Finally, as well as assuring physicians that their patients will be safer and more compliant when taking existing drugs, Eyenovia’s approach could open the door to products that – because of toxicity issues – are currently not approved in eyedrop form. “There is Level 1 evidence for atropine slowing the progression of myopia in children by 60 percent (3). However, we haven’t been able to prescribe atropine eye drops because of their side effects. The option of accurate microdosing completely changes this situation,” says Ianchulev. “Small, precise doses may eliminate eye-drop toxicities and turn an unacceptable drug into a tolerable product.”

- Piezo-print technology in a handheld device allows ocular drug delivery in precise 6-8 microlitre volumes
- Exposure to formulation-related irritants is decreased by 80 percent – while retaining a biological effect equivalent to that mediated by eye-dropper delivery
- The technology is applicable to monotherapy products and to drug combinations, and is anticipated to reduce side effects and improve compliance
- Indications include large markets: adult glaucoma, office-based dilation, and pediatric patients, such as premature infants and children with myopia (prevalence: 5 million)
- The device is in Phase III trials in three indications: microdosed latanoprost for chronic angle-closure glaucoma, microdosed atropine for prevention of myopia progression in children, and microdosed phenylephrine/tropicamide for eye dilation.
Room to grow
However innovative the technology, for a company to survive, the objective must also make commercial sense – a point not lost on Eyenovia. Potential markets for the technology are large, and include not only adult glaucoma and pediatric myopia patients, but also the 80 million patients in the US alone per year who undergo dilation in the doctor’s office – and suffer stinging or burning eyes from the preservative and the dual overdose, since doctors often use two agents simultaneously to dilate the pupil (tropicamide and phenylephrine) (4). “Eyenovia microdosing delivers the same therapeutic benefit as eye drops, but much more mildly – in a high-precision single microdose of a fixed co-formulation of the two drugs,” says Ianchulev. He adds that the improved safety associated with controlled microdoses suggests that GPs could start administering drugs that previously were only provided by specialist ophthalmologists, making patient management more straightforward and cost-effective. Ultimately, however, Ianchulev sees the technology as far more than just a means of enabling delivery of third-party drugs; the company is building a pipeline of proprietary formulations, including three products in Phase III – for mydriasis, myopia and chronic angle closure glaucoma – and one in Phase I for dry eye.
And the longer-term aim? Ianchulev has set his sights high: nothing short of resolving the world’s myopia problem… In the meantime, he’ll settle for lower side effects and a transformation in adherence monitoring. If Eyenovia’s tech does end up being disruptive, what of the loser? Well, when compared with piezo-electric Bluetooth-enabled microdose delivery, the humble eyedropper starts to look like something not just from a previous century, but from the dark ages!
References
- 1. R Gupta, B Patil et al., “Evaluating eye drop instillation technique in glaucoma patients”, J Glaucoma, 3, 189-192 (2012). PMID: 21336146 Y Shirasaki, “Molecular design for enhancement of ocular penetration”, Journal of Pharmaceutical Sciences, 97, 2462-96 (2008). PMID: 17918725 SL Pineles, RT Kraker et al., “Atropine for the Prevention of Myopia Progression in Children: A Report by the American Academy of Ophthalmology”, Ophthalmology, 124, 1857-1866 (2017). PMID: 28669492 AAO, “The State of the Optometric Profession: 2013” (2013). Available at: https://tinyurl.com/yclgxhst. Accessed November 19. 2018.
