- Femtosecond laser-assisted surgery has no clear advantages over manual cutting so far.
- In astigmatic keratotomy (AK) ,incisions of uniform depth overcorrect at the center and under-correct at the ends of the incision.
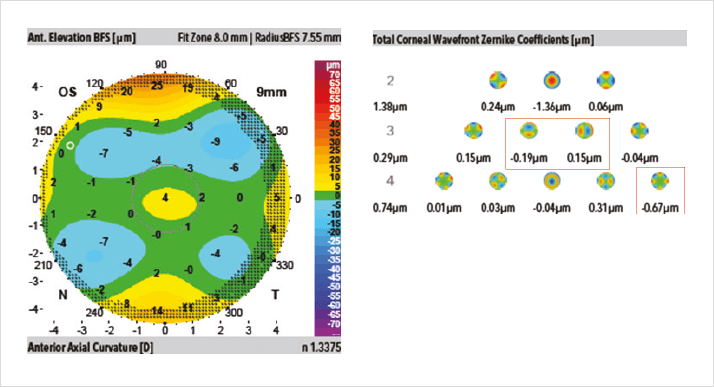
- This results in unwanted higher order aberrations like new oblique astigmatism, tetrafoil and coma.
- Laser Bridge AK with a femtosecond laser has the potential to minimize these problems by varying the depth of incision at different points.
The value of femtosecond laser surgery in ophthalmology is controversial. Some ophthalmologists appreciate the automated, precise and highly reproducible incisions that the lasers perform but other surgeons argue that femtosecond lasers don’t do anything better than manual instruments and, at over $500,000 (€370,000), they are simply considered expensive toys. Currently, there is no femtosecond laser “killer application” that would make it a completely compelling choice over the manual alternative. This may soon change.
The value of femtosecond laser surgery in ophthalmology is controversial. Some ophthalmologists appreciate the automated, precise and highly reproducible incisions that the lasers perform but other surgeons argue that femtosecond lasers don’t do anything better than manual instruments and, at over $500,000 (€370,000), they are simply considered expensive toys. Currently, there is no femtosecond laser “killer application” that would make it a completely compelling choice over the manual alternative. This may soon change. Femtosecond lasers can be used to perform astigmatic keratotomy (AK) – and there may be benefits associated with their use. In AK, the laser can be used to perform intrastromal incisions (the cuts are made in the stromal layer, sparing the corneal surface) and this may help reduce postoperative pain and infection risk. Visual outcomes, however, are no better than what can be achieved by hand, and an intrastromal incision adds the risk of some future surgeon creating a flap and precipitating massive astigmatism as the intrastromal incisions effectively become penetrating.
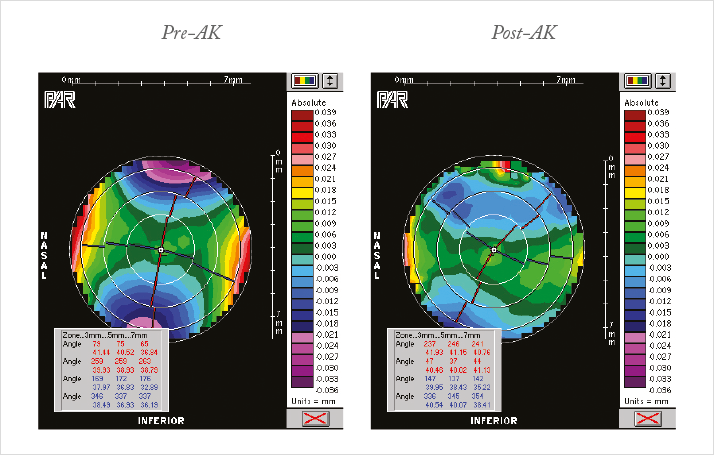
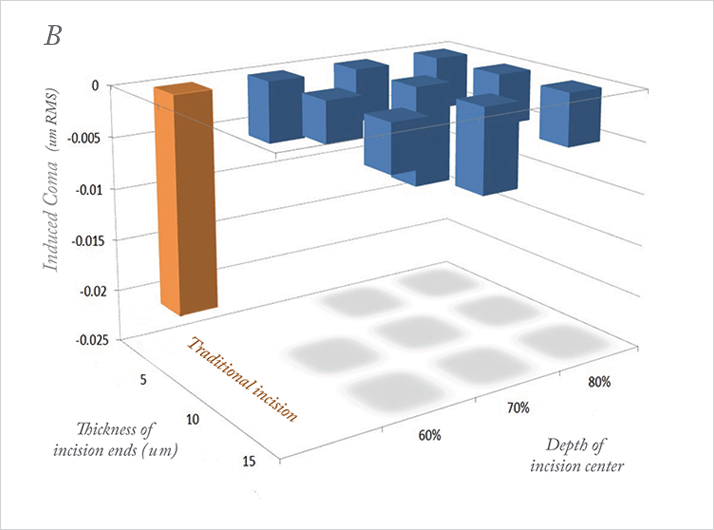
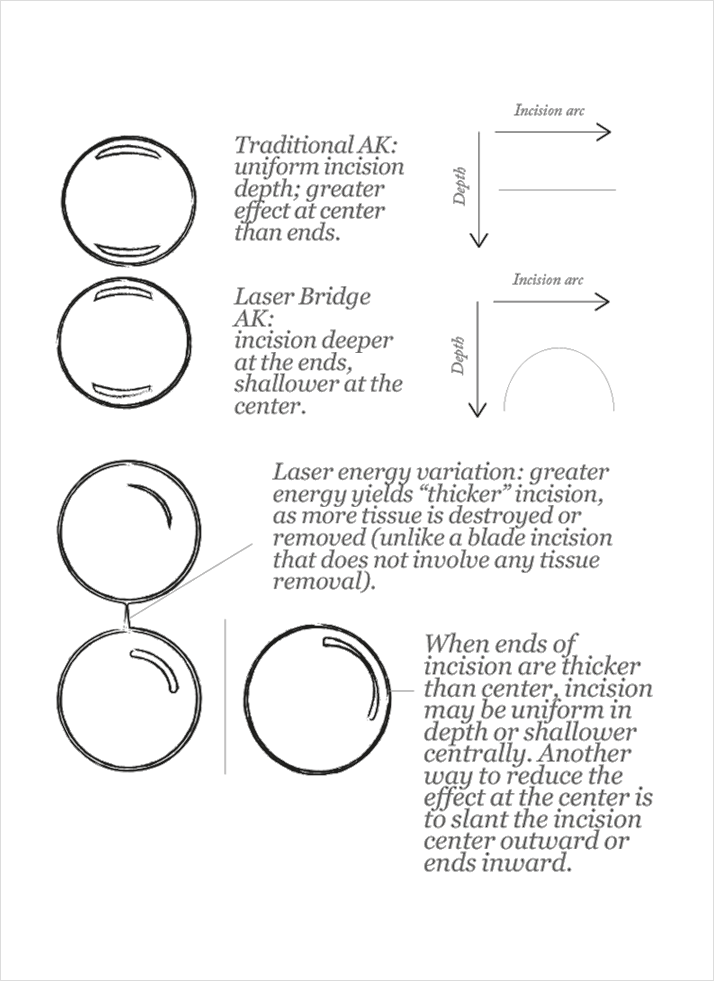
Whether the incisions are manual or performed with femtosecond lasers, AK has a greater effect at the center of the cornea than at its ends. This is something that we commonly observe on elevation maps. Because the ends of any corneal incision are stabilized by intact cornea, the center is the point of greatest relaxation. Essentially, this means that incisions of uniform depth create a greater effect in the center and less at the ends (Figure 1). Overcorrection in the center of an AK induces new astigmatism at an oblique axis, tetrafoil and coma (Figure 2), so it’s important to minimize these effects wherever possible.
The number of variables at play make AK a difficult procedure to predict and perfect. The incisions have their greatest effect when they are longer, deeper, within a smaller optical zone, or when performed in an older patient with a more rigid cornea. Femtosecond lasers perform incisions of uniform depth and optical zone, yet issues that dog manual cutting with a diamond blade persist. The greatest challenge is optimizing for the most predictable and maximally corrective optical effects, with the least amount of aberration. Canrobert Oliveira and others have tried to solve this by adding additional incisions but these can also have unwanted effects (1). We have an alternative solution.
Laser Bridge AK
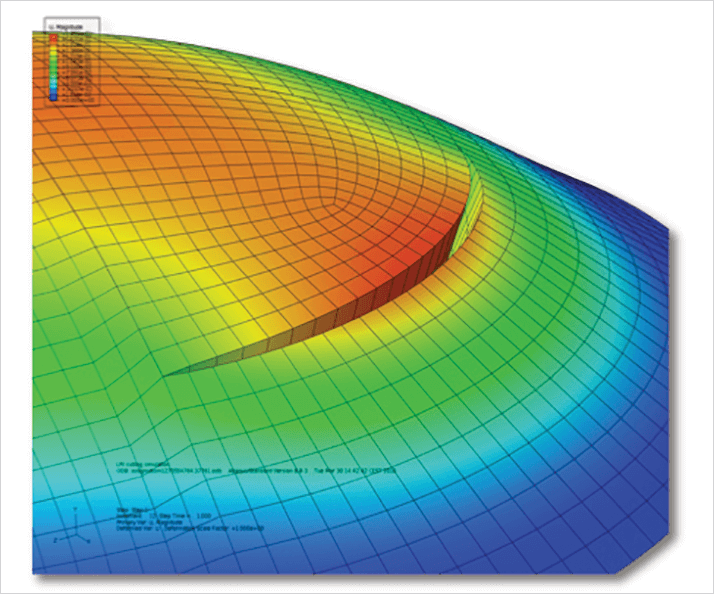
We increase the astigmatic effect of the ends of the incision by making them deeper and diminish the astigmatic effect of the center of the incision by making it shallower (see Box). This serves two functions. First, it mitigates the overcorrecting effect of the center of the incision and second, it augments the corrective effects of the ends. This technique, termed Laser Bridge AK, is possible only with a suitably-programed femtosecond laser systems. Femtosecond lasers also open up the possibility of varying the incision thickness. While blade incisions do not remove tissue, femtosecond lasers do so via ablation, with the amount ablated being programmable. More tissue can be ablated in one area than another, and other parameters can be varied too. For example, the laser can perform an incision that is thicker at its ends than at the center, whether the incision has uniform depth or is shallower at the center. It can even be programed to make the center of the incision slant outward, and the ends slant inward, to further manipulate their relative effect.It is crucial that we establish an optimal cutting pattern for a given patient, given the myriad possibilities. The first step is computer simulation. We undertook a virtual clinical study that compared our proposed AK incision architectures to standard AK, determining the astigmatic effect and higher order aberrations (HOAs) generated by both approaches. This was done using finite element modeling with Optimeyes software, to simulate femtosecond laser arcuate corneal-relaxing incisions on patient-specific corneal models (Figure 3). This modeling takes into account realistic fiber distribution from x-ray scattering, and recognizes that corneal stroma is denser anteriorly than posteriorly. We presented the data from this study at the 2014 Association for Research in Vision and Ophthalmology annual meeting in Orlando, FL, USA (2).
We compared incisions (30° in length, made at the 8 mm optical zone) of uniform depth and thickness with AKs that had incision ends that were deeper, thicker, or deeper and thicker than the incision center. Two measures were assessed: astigmatic effect and induced HOAs. What we found was that thicker ends/ shallow center Laser Bridge incisions reduced spherical aberration relative to traditional AK incisions (Figure 4a). As for HOAs, all forms of Laser Bridge incisions reduced trefoil by 81 percent, and coma – the most visually significant HOA – by 82 percent, compared with traditional uniform AK (Figure 4b).
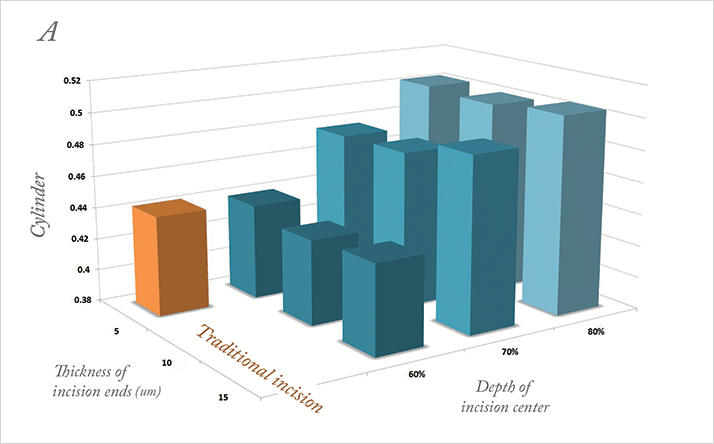
But what about the correction of astigmatism? Do incisions shallower in the center result in less correction of astigmatism? We found that most Laser Bridge incision types actually yield a 15 percent greater astigmatic correction compared with a traditional incision, even though they induce fewer HOAs. So, in simulation, at least, Laser Bridge incision produces better correction of astigmatism, with far fewer HOAs like coma, spherical aberration, trefoil, and tetrafoil. The results of the simulation remain to be validated clinically, but it is possible that femtosecond laser can improve unaided and best spectacle-corrected visual acuity. It may be the first “killer application” for femtosecond lasers in ophthalmology. Anita Nevyas-Wallace is a cataract and refractive surgeon at Nevyas Eye Associates, Bala Cynwyd, PA, USA.
AK incisions made possible with femtosecond lasers
References
- G.D. Freitas, “Limbal Relaxing Incision with Inverse C Procedure”, Film F88, ASCRS Annual Meeting, Chicago, April 4–9 (2008). A. Nevyas-Wallace, C.J. Roberts, H.P. Studer, “Effect of Novel Architecture for Femtosecond Laser Astigmatic Keratotomy (AK) on Induced Aberration on Patient-Specific Computational Modeling”, IOVS, 55, ARVO E-Abstract 1553 (2014).
