- Wavefront aberrometers quantify higher order aberrations objectively.
- The problem with being objective is that we do not see with our optical system, we see with our brain.
- Point Spread Function (PSF) refractors provide subjective corrections that optimize images on the retina.
- Pre-operative aberrometry with PSF optimizes refractive outcomes following LASIK or PRK surgery.
Wavefront aberrations are optical imperfections of the eye that prevent light from focusing flawlessly on the macula, resulting in a less than perfect image being perceived by an individual. Lower-order aberrations, including myopia, hyperopia and astigmatism, are common and easily corrected with spectacles, contact lenses or refractive surgery. Higher-order aberrations (HOAs), which are of the third order and above, are more complex vision errors that cannot be easily corrected (1). Examples of HOAs are coma, spherical aberration and trefoil. They can lead to symptoms such as difficulty with night vision, glare, halos around bright lights, blurring, starburst patterns, or diplopia (1).
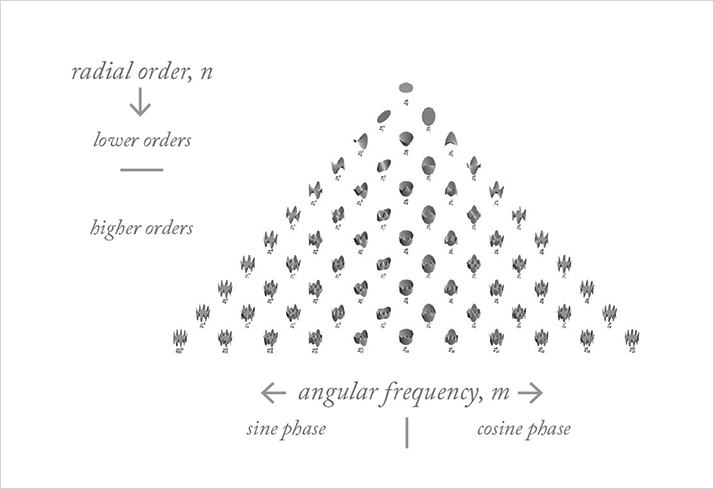
Although patients may still be able to read and see objects at a distance, HOAs can dramatically affect overall quality of vision, particularly in low lighting conditions. Traditionally, clinicians have relied on patients’ subjective reports to identify HOAs, but in recent years, wavefront aberrometers have been introduced to assist with diagnosis and measurement. Aberrometers measure the distortion of light as it passes through the eye’s optics (1). This information is expressed as a mathematical estimation called the Zernike polynomial expansion, which describes the degree of distortion present in the eye (Figure 1). These distortions can be measured either as a total amount (that is, the root mean square [RMS] error), or individually. Ultimately, it is the point-spread function (PSF), which is the smallest point of light that one’s eye can resolve, that indicates the level of vision capability; based on this, we can extrapolate an estimate of the level of aberrations.
The PSF Refractor
The PSF Refractor assesses the ultimate level of resolution capable for each patient – the PSF – and works to provide an improved subjective refraction. The main disadvantage with older ways of measuring wavefronts is that they are truly objective – they measure distortions by sending a beam of infrared light through the cornea, through the lens, through the vitreous, off the retina, and back again, measuring changes from the wavefront going in versus going out. While this describes differences as higher-order aberrations, the problem is that it is wholly objective, whereas we do not see with our optical system, we see with our brain and there are patients in whom that correction does not compute very well in that organ. This can result in a lot of inaccuracy. The PSF Refractor overcomes this problem as it relies on the most important image: the resolution of a point of light on the retina. This is a subjective measurement that can then be used to optimize that image: the patient gets an subjective refraction, and clinicians can correct for all higher-order aberrations so that each patient gets their ideal visual prescription (see “An Invaluable Tool” below). Rather than correcting perceived aberrations and putting it into a spectacle lens, all of the aberrations, including low-order and high-order, are assessed to obtain the optimal prescription – the PSF Refractor provides a tighter level of correction. The current manual phoropter has a range of ± 0.25 diopters (D) and while this level is suitable for a large percentage of patients, many patients have a resolution that is different from this value, often much lower.The maximum resolution is far finer than 0.25 D and some patients (for example, young patients or athletes) can resolve a much smaller range of bracketing. Now we have free-form lens technology, which allows corrections to a fine resolution. This particularly benefits patients with night vision refinement. Using the PSF Refractor, we can show patients – with one click of a button – the prescription prior to and after measurement. This immediate comparison allows a decision on whether there is enough improvement to warrant the next step. Our group recently compared the performance of the PSF Refractor with that of a traditional phoropter (2). The study included the right eyes of 30 patients (mean age 37.3 years; range 10−68 years) who presented for a routine visual examination. Each patient underwent subjective refraction, first with a standard phoropter with binocular refraction using +1.0 D fogging in the fellow eye, and binocular balancing at the finishing; and monocular refraction with the PSF Refractor, without binocular balancing. The manifest refraction and visual acuity measured with each method were recorded.
In 70 percent of patients, the spherical equivalent (SE) obtained with the PSF Refractor was within 0.13 D of that obtained with a binocularly balanced phoropter. In 27 percent and 3 percent of patients, respectively, the SE differed by more than 0.13 D and 0.26 D. In terms of visual acuity, in the majority of patients (93.5 percent), the results obtained with the PSF Refractor were equal to or better than those obtained with the phoropter binocular method (2). Our study indicates that the PSF-based refractor provides accurate manifest refraction and visual acuity readings without the need for binocular balancing. Consequently, subjective refraction is a simpler and faster process.
Clinical experience with the PSF Refractor
The PSF Refractor provides two advantages in terms of optimizing vision. One, it helps patients who complain of shadows to images, double vision, lack of crispness, lack of color perception, night driving problems, halos or coma. Two, it increases efficiency in the clinic. Because it does not require binocular testing, simply because the endpoint is so well-defined for each eye, a quick measurement ensures that we are not over-correcting; even this is not necessary if you show the patient the Snellen chart through the VMax PSF Refractor. A final advantage; patients are considerably less stressed doing this type of refraction compared with what they had to undergo in the past.Paul M. Karpecki is an Optometrist at the Koffler Vision Group, Lexington, KY, USA, and David Geffen is an Optometrist at the Gordon-Weiss-Schanzlin Vision Institute, La Jolla, CA, USA.
An Invaluable Tool
By Stephen Hollis The PSF Refractor is one of the most important tools that I have integrated into my practice in recent years. Since late 2013, my team, which specializes in refractive surgery, has performed over 2,000 examinations with the device, before going on to perform LASIK or PRK. Because the PSF Refractor is based on point spread (a way of measuring wavefront error), you can get improvements in refraction if you’re using a laser that does not have wavefront technology. It’s more accurate than the traditional phoropter because it measures in increments of 0.05 D. This is important because the laser machine I use also operates in increments of 0.05 D. Additionally, with a standard phoropter it’s very difficult to measure the vertex distance; consequently, no one does it despite the fact that the vertex distance affects LASIK outcomes, particularly in patients with a high refractive error. This device refracts with a zero vertex, right on the cornea. Although my laser machine is set at 13.75 (which is the average vertex distance), I can set the PSF refractor to output data at 13.75, so I am getting much better outcomes for a patient with, say a -9.0 D prescription, than ever before. I’ve also been able to achieve 20/15 vision in more or my LASIK patients, something I wasn’t able to do with the traditional phoropter. For a refractive surgeon, this device is a revelation. Stephen Hollis is an ophthalmologist working in private practice at Hollis LASIK in Auburn, Alabama, USA.References
- M. Resan, M. Vukosavljević and M. Milivojević (2012). Wavefront Aberrations, Advances in Ophthalmology, Dr Shimon Rumelt (Ed.), InTech, Available here.
- P.M. Karpecki and D. Geffen, poster presentation given at the EastWest Eye Conference, October 3–6, Cleveland, OH, USA, (2013).
