- We start by locating the scleral spur’s base, which in most cases will be evident, or will become visible behind or right next to the trabecular meshwork, after an initial minimal blunt dissection of its base
- (video available at: http://top.txp.to/mp-ss).
- We continue by using a toothed forceps to apply countertraction to the edge of the corneoscleral rim and a second toothed forceps (preferably 0.12 mm) to tightly grab the scleral spur deep into the sclera (Figure 2a), and gently apply perpendicular traction on the Z-axis.
- This traction creates a focal disinsertion of the scleral spur from the sclera (Figure 2b)
- This is then further extended circumferentially (Figure 2c) using both toothed forceps, one for traction, the other for countertraction.
- In most cases, the entirety of the circumferential scleral spur ring will dissect out as a single “snake-like” strip, 360 degrees around (Figure 2d–e).
- If the scleral spur strip happens to break, the dissection can be continued by regrasping the scleral spur where the break occurred, until the full circumference is disinserted. It is very important that you see a white stripe of tissue disinserting from the corneoscleral rim, since one can mistakenly disinsert the iris root, which would
- not accomplish the goals of
- our technique.
- Once the scleral spur is removed, the plane of dissection of our DMEK donor tissue is revealed (Figure 2f), as we have removed its main adhesion to the scleral rim, and this can be found anteriorly adjacent to our initial dissecting plane, in a configuration that resembles the inferior free edge of a curtain hanging from a wall.
- This edge can be lifted and gently pulled anteriorly, in order to continue with our standard approach, using the Rootman-Goldich modified Sloane’s LASEK micro hoe to further anteriorly dissect the trabecular-E-DM junction.
- This breaks the only remaining main hurdle for our donor dissection, Descemet’s insertion at the level of Schwalbe’s line, and allows us to continue the disinsertion of the E-DM complex from the stromal bed.
- Luckily, this second attachment at Schwalbe’s line is not as strong, creating less resistance to dissection and generating far less radial tension.
- At this point, you can gently push the membrane centrally, instead of actively scraping the insertion to break it (as was done for the scleral spur attachment using the original technique).
can deliver great outcome
- DMEK can deliver great outcomes in corneal endothelial transplantation, but the learning curve can be steep
- David Rootman from the University of Toronto cleverly modified Gerrit Melles’ original technique for donor tissue preparation, and his method has seen success in many cases – but going through the learning curve remains a challenge for some
- This new modification, known as scleral spurectomy, involves scleral spur disinsertion to facilitate peripheral blunt dissection of the trabecular-endothelium-Descemet’s membrane complex, decreasing the risk of tears which can compromise donor endothelial tissue viability
- Scleral spurectomy is easy to learn, can reduce the number of possible complications during the dissection process, and is likely to be useful for surgeons who don’t have access to pre-stripped DMEK donor grafts
- DMEK can deliver great outcomes in corneal endothelial transplantation, but the learning curve can be steep
- David Rootman from the University of Toronto cleverly modified Gerrit Melles’ original technique for donor tissue preparation, and his method has seen success in many cases – but going through the learning curve remains a challenge for some
- This new modification, known as scleral spurectomy, involves scleral spur disinsertion to facilitate peripheral blunt dissection of the trabecular-endothelium-Descemet’s membrane complex, decreasing the risk of tears which can compromise donor endothelial tissue viability
- Scleral spurectomy is easy to learn, can reduce the number of possible complications during the dissection process, and is likely to be useful for surgeons who don’t have access to pre-stripped DMEK donor grafts
Since it was first described 17 years ago (1), Descemet Membrane Endothelial Keratoplasty (DMEK) has become a popular and widely-accepted technique in the cornea community. But despite its clear advantages in terms of visual results and rejection rates (2), its adoption has not been widespread in some areas worldwide. Why? The technique has a steep learning curve, mostly due to donor tissue preparation. Donor cornea tissue is a precious resource; in countries with limited availability, many surgeons might opt to persist with full-thickness grafts rather than risk donor corneas during the DMEK learning curve. Is there a better way? Multiple different techniques have been described for donor tissue preparation (3–5), all with the aim of standardizing the steps that are needed to achieve a suitable endothelium-Descemet’s membrane (E-DM) complex to restore endothelial function. We describe another here.
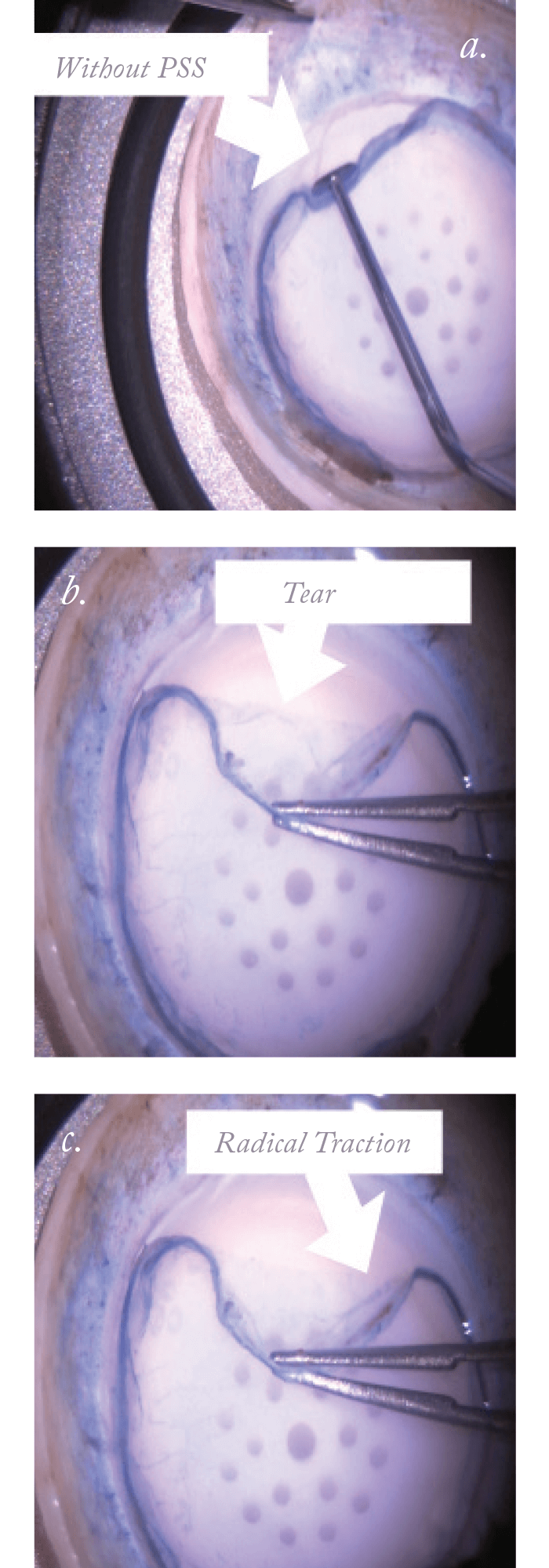
Getting ahead of the learning curve
We were all trained to perform DMEK under David Rootman’s supervision at the University of Toronto. Everything we know about this technique, we owe to his generous teaching. His standard technique for donor tissue preparation (6) brilliantly modifies the original Melles technique (3), and starts with a blunt dissection of the trabecular meshwork on a corneoscleral rim using a Rootman-Goldich modified Sloane’s LASEK micro hoe (Katena Products). It involves careful dissection of the peripheral trabecular insertion from the scleral spur, and continues anteriorly, freeing the trabeculo-Descemetic junction from its insertion at Schwalbe’s line, and then the E-DM complex from its stromal attachment. This technique has been used successfully in more than 300 cases – but it’s not without challenges. It still involves a learning curve, and can still present problems with some donors. These include: difficulty finding the correct plane of dissection by dissecting either behind or in front of the scleral spur (sometimes including the dissected spur into the membrane complex), the creation of one or multiple adhesive tags between the scleral spur and the E-DM complex (Figure 1a), and the creation of radial or circumferential tears (that generally tend to extend centrally) during the initial dissection of the internal aspect of the trabecular meshwork from the scleral spur (Figure 1b). These tears can be explained by the radial or para-radial vector force that results from the centripetal force that’s applied by the surgeon to free the membrane from its insertion, and the force applied from the scleral spur insertion itself at the spot right next to the dissected area (Figure 1c). Although these challenges can usually be overcome by an experienced surgeon, it can be difficult to survive the learning curve and become confident using this technique, especially when every donortissue counts. Two main attachments of the donor endothelium need to be broken for a successful peripheral dissection before starting the standard stripping motion. One is the external, strong and thick attachment at the level of the scleral spur, and the second one is a relatively loose and anterior attachment at the level of Schwalbe’s line. We call this new technique of scleral spur disinsertion to facilitate peripheral blunt dissection of the trabecular-E-DM complex “Scleral spurectomy” (see Sidebar, “Taking a Technique From the Lab to the OR”).
- We start by locating the scleral spur’s base, which in most cases will be evident, or will become visible behind or right next to the trabecular meshwork, after an initial minimal blunt dissection of its base (video available at: http://top.txp.to/mp-ss).
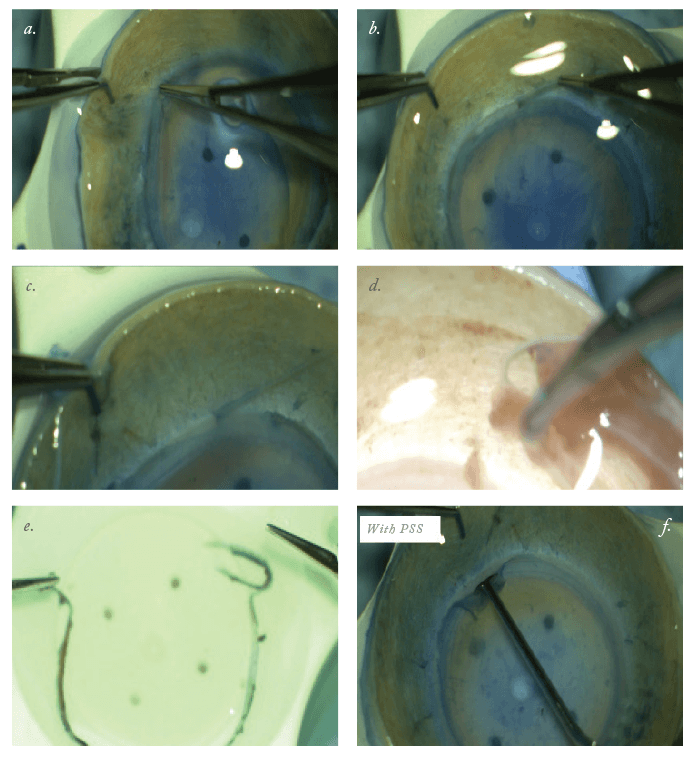
- We continue by using a toothed forceps to apply countertraction to the edge of the corneoscleral rim and a second toothed forceps (preferably 0.12 mm) to tightly grab the scleral spur deep into the sclera (Figure 2a), and gently apply perpendicular traction on the Z-axis.
- This traction creates a focal disinsertion of the scleral spur from the sclera (Figure 2b)
- This is then further extended circumferentially (Figure 2c) using both toothed forceps, one for traction, the other for countertraction.
- In most cases, the entirety of the circumferential scleral spur ring will dissect out as a single “snake-like” strip, 360 degrees around (Figure 2d–e).
- If the scleral spur strip happens to break, the dissection can be continued by regrasping the scleral spur where the break occurred, until the full circumference is disinserted. It is very important that you see a white stripe of tissue disinserting from the corneoscleral rim, since one can mistakenly disinsert the iris root, which would not accomplish the goals of our technique.
- Once the scleral spur is removed, the plane of dissection of our DMEK donor tissue is revealed (Figure 2f), as we have removed its main adhesion to the scleral rim, and this can be found anteriorly adjacent to our initial dissecting plane, in a configuration that resembles the inferior free edge of a curtain hanging from a wall.
- This edge can be lifted and gently pulled anteriorly, in order to continue with our standard approach, using the Rootman-Goldich modified Sloane’s LASEK micro hoe to further anteriorly dissect the trabecular-E-DM junction.
- This breaks the only remaining main hurdle for our donor dissection, Descemet’s insertion at the level of Schwalbe’s line, and allows us to continue the disinsertion of the E-DM complex from the stromal bed.
- Luckily, this second attachment at Schwalbe’s line is not as strong, creating less resistance to dissection and generating far less radial tension.
- At this point, you can gently push the membrane centrally, instead of actively scraping the insertion to break it (as was done for the scleral spur attachment using the original technique).
This method was initially applied to 30 consecutive donor corneoscleral rims at the lab at the University of Toronto, before moving to the operating room. Since then, we (and several other surgeons) have fully converted to it for the past year and a half. It has already been presented in our DMEK Course at the ASCRS and ESCRS meetings, and is currently part of the surgical toolkit that we teach to cornea surgeons in training.
Do it yourself
The main advantages we’ve found with this technique include less difficulty in finding the correct dissection plane, as removing the scleral spur essentially eliminates the anterior versus posterior to the scleral spur dissection dilemma. Since the scleral spur is not there anymore, it eliminates the adhesive tags between the scleral spur and our dissected membrane, which in the standard technique, needed to be commonly cut with Vannas scissors for a successful dissection. Furthermore, it eliminates the radial or para-radial force vector created by the scleral spur insertion during centripetal dissection with the micro hoe, which results in a reduced likelihood of creating radial or circumferential tears that might compromise the viability of our donor endothelial tissue button. We have yet to see a peripheral tear during dissection using this technique. Scleral spurectomy can be especially useful for the newer DMEK surgeon, since it reduces the amount of possible complications during the dissection process, which a more experienced surgeon could most likely manage. In our experience, we believe it is a very quick, easy to learn, reproducible and effective technique which has the potential to decrease the rate of donor tissue tears if you are experiencing them, and helps in the management of friable corneal tissue, especially for surgeons that do not have access to an eye bank that can pre-strip DMEK donor grafts and require self-prepared tissue, as is the case in most parts of the world. We hope that this scleral spur dissection/stripping technique will help to popularize DMEK among cornea surgeons, and make tissue preparation a less daunting process.References
- GRJ Melles et al., “Transplantation of Descemet’s membrane carrying viable endothelium through a small scleral incision” Invest Ophthalmol Vis Sci, 39, S76, Abstract no. 343 (1998). M Price et al., “Descemet’s membrane endothelial keratoplasty prospective multicenter study of visual and refractive outcomes and endothelial survival”, Ophthalmology, 116, 2361–2368 (2009). PMID: 19875170. JT Lie et al., “Donor tissue preparation forDescemet membrane endothelial keratoplasty”,J Cataract Refract Surg, 34, 1578–1583(2008). PMID: 18721723. F Kruse et al., “Stepwise approach to donor preparation and insertion increases safety and outcome of Descemet membrane endothelial keratoplasty”, Cornea, 30, 580–587 (2011). PMID: 21598430. P Veldman et al., “Stamping an S on DMEK donor tissue to prevent upside-down grafts: laboratory validation and detailed preparation technique description”, Cornea, 34, 1175–1178 (2015). PMID: 26147839. D Rootman, “Blunt dissection for DMEK donor tissue preparation using a microhoe”. Presented as part of the “DMEK from D to K” course at the ESCRS Meeting in Barcelona, 2015 and the ASCRS Meeting in New Orleans, 2016.
