When it comes to discussing femtosecond laser-assisted cataract (FLACS) surgery with your patients, a good comparison is the Texas Two-Step. It’s a dance, with a leader and a follower; you have to take the lead and guide patients through the process. Doing so requires confidence in the technology (and this is easy with the FEMTO LDV Z8). If you and your staff believe in the technology, your patients will too. But confidence is just the opening move – the most important step is patient education. It starts from the front – advertising, putting the procedure on the front page of your website, and crucially, having your referral network discuss femto cataract surgery with their patients. If people are asking about FLACS technology before they even turn up to your office, you’re already ahead. It’s also essential to educate your staff thoroughly. If a patient presents for cataract surgery and they have some astigmatism, my staff will say: “You’ve got astigmatism, do you know what that is? Have you thought about correcting that?” The conversation starts right from the door. When I have that initial conversation with the patient, I use phrases that I think help them understand the technology: “A computer measures your unique eye shape,” “this technology adapts to your unique eye shape,” and “this is blade-free surgery” – are all phrases patients like to hear, as is describing the laser as “extremely precise,” which is greatly reassuring.
Consider making educational videos. Explaining all of the available lens and laser options can eat up your time quite quickly, but a video helps prepare the patient before they see you. When describing the procedure, I show them FLACS with the perfectly centered laser capsulotomy. It makes the patient understand exactly what you’re offering and the value of it, and this is what converts most people right there and then. It’s really important to avoid selling the technology to patients, though. I just want my patients to be as knowledgeable as possible about the procedure, so they can make their own choice – I never pressure them into a decision. It’s fine for them to go away and discuss it with their friends and family, but make sure you have someone available that can answer any follow up questions. But when I’m asked “What should I choose, doctor?” I say this: “I’m very comfortable with traditional surgery by hand, that’s what I still do the majority of the time. But, with that said, I am not as precise as the laser and it’s a nice option for those who choose it.” If I feel I can joke with the patient, I might say something like, “I don’t want you to sell your left kidney to do this if that’s what it would require,” but note that “there are benefits to laser”, and (because I’m based in Texas) I’ll add “… especially if we’re placing one of these fancy lenses.” You might want to customize that text, but it’s served me well. Good luck!
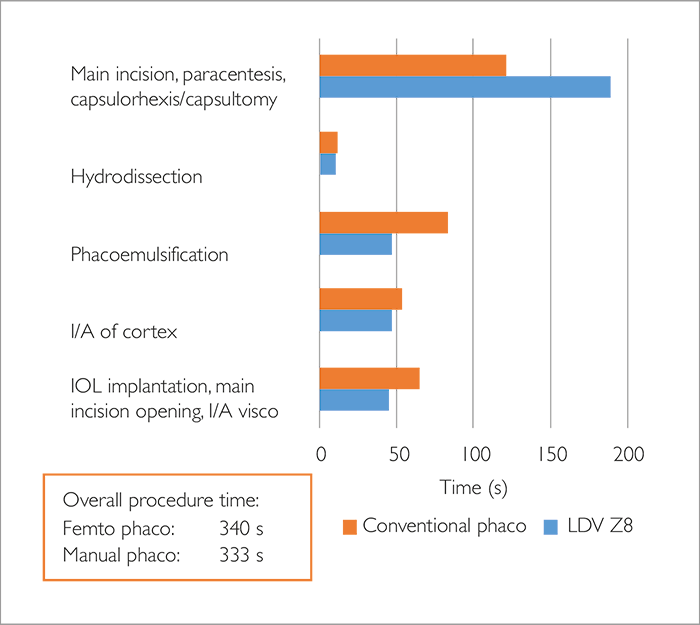
One of the commonest misconceptions of FLACS is that it takes far longer to perform than manual surgery. I want to show you that, with a well-organized and prepared team, and the right instrument, that simply isn’t the case.
To demonstrate this, I performed a study that involves 131 patients, with 68 undergoing FLACS with the Ziemer FEMTO LDV Z8 and 63 undergoing the manual surgery. Baseline demographics in both groups were similar, with mean ages of 70.1 ± 8.2 years in the femtosecond laser-treated and manual surgery groups, respectively – although the cataracts in the FLACS group were significantly harder than in the traditional surgery group. We measured the time involved in each step of the procedure, and found the overall procedure time to be only 7 seconds longer with FEMTO LDV Z8 than with manual phaco (Figure 1). How can this be? There are three main areas where you gain time with the Z8. The first is the quality of the cut it makes for the main and side port incisions – compared with manual incisions they are faster to make and induce less astigmatism. I find that I often have to reopen manual incisions to implant the IOL – I don’t when they have been made with the laser. Another is the efficiency of lens fragmentation. Even in patients with Grade 4 cataract, the fragmentation of the lens is rapid and effective, and this translates into fast and efficient phacoemulsification, and shorter effective phacoemulsification times. When it comes to workflow, the fact that the Z8 (unlike all other femtosecond lasers on the market) can be wheeled to and from the patient during the procedure means that, for all intents and purposes, the workflow is the same as traditional manual cataract surgery: a single working position, with no patient movement, saving time. Ultimately, with a well-organized and prepared team, with the Z8 at least, you can combine high volume cataract surgery with femtosecond lasers.
Finally, the advanced optics of the Z8, using its liquid interface mean that you can make incredibly precise arcuate incisions. My experience is that the arcuate incisions have been precise in position and depth, and the software has been particularly easy to use for both the planning and the execution of the incisions. In terms of cataract surgery, as this laser can be used to create arcuate incisions as part of an astigmatism control strategy, it can provide an excellent alternative to toric IOLs in many cases.
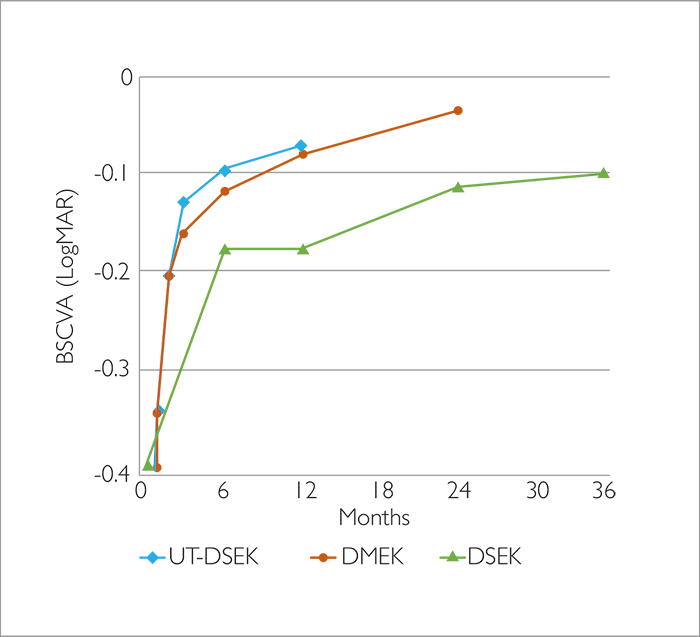
The last 20 years has seen a substantial move away from penetrating keratoplasty (PK) towards lamellar keratoplasty, in particular towards Descemet Stripping Endothelial Keratoplasty (DSEK) and Descemet membrane endothelial keratoplasty (DMEK). Both procedures have pros and cons: DMEK provides better visual outcomes and a faster recovery than DSEK, but tissue loss and graft detachment rates are higher, and it’s a lengthy, challenging procedure with a sharp learning curve. Could DSEK be improved to match DMEK’s outcomes? In 2011, Neff et al. (1) showed that the visual results from DSEK surgery depend very much on the lamellar thickness – they found that if it was ≤130 µm, this translated into BSCVA >0.8 in 100 percent of patients, and 1.0 in 71 percent. If the thickness was >130 µm, BSCVA was >0.8 in 50 percent, and only 19 percent of patients achieved a BSCVA score of 1.0. This raised the concept of ultra-thin (UT)-DSEK grafts, something that promised the “best of both worlds”. It’s not that simple; the preparation of UT-DSEK grafts requires at least one, and maybe two microkeratome passes – and the graft thicknesses they produce can vary from what was intended. I like to describe microkeratome-produced grafts as “dog-eared” – they’re thinner in the center and thicker in the periphery. Because the outer surface is the reference plane, you always end up with sharp edges. Further, the endothelial cells try to cover these “open doors” – they migrate out around the edge of the graft, and the graft falls off. Finally, these grafts last for an average of 10 years before needing to be replaced.
UT-DSEK video methods showcase
View the UT-DSEK video methods showcase here
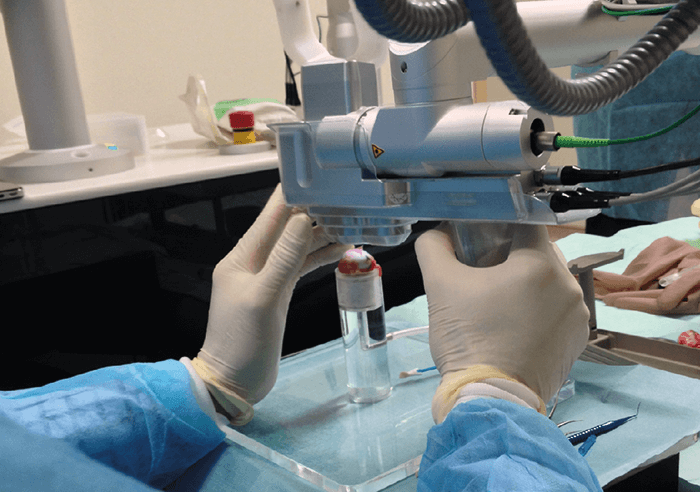
The question is: can we create better UT-DSEK grafts using a femtosecond laser? For most systems, no. High-energy laser systems create large cavitation bubbles that would burst through the layers of the cornea, and cause too much damage. What’s required is an extremely precise, low-energy laser system, with a high repetition rate and overlapping spots that provide the precision required for such delicate laser dissections – and help avoid leaving tissue bridges that can lead to tears. This is exactly what the FEMTO LDV Z8 provides. My preferred method for creating a very precise UT-DSEK graft is detailed in a video methods showcase (at bit.ly/ZiemerZ8), but the femtosecond laser dissection step is simple – it involves mounting the donor cornea upside down in the Ziemer artificial anterior chamber, and applying 60 cmH2O of pressure and applanating the cornea to the interface using hyaluronic acid as the contact medium to avoid damage to the endothelium. The pocket we create with the laser has two entrances, which is helpful for manual preparation. The laser is removed, then I proceed as described in the methods video. You might wonder if all this manipulation leads to more endothelial cell loss relative to microkeratome-produced UT-DSEK grafts: the answer is no. Further, the grafts don’t fall off, like they did with PK, and there’s only a very slight trend towards lower endothelial cell counts over the years. Finally, Figure 2 shows that the visual outcomes we’ve seen with UT-DSEK are very comparable to the DMEK results. So my overall message: UT-DSEK works using the femtosecond laser.
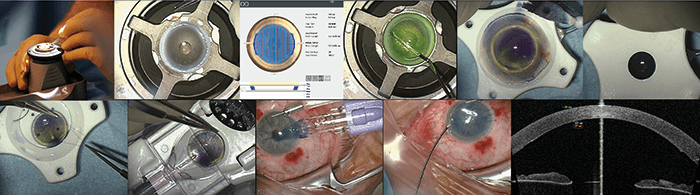
We all know the gold standard for pterygium surgery is a conjunctival autograft – and the most difficult part of the surgery is harvesting the conjunctival graft. There is a significant learning curve in obtaining adequate graft size with minimal sub-Tenon tissue, and surgical experience influences both success and complication rates. Pterygium recurrence rates are lower in experienced surgeons, presumably because more experienced surgeons harvest thinner grafts. If the problem is the learning curve, the challenge is to make the graft harvesting outcomes as optimal and as reproducible as possible for every surgeon. We tested the feasibility of using the Z8 to harvest the grafts, in a process we call FLAPS: femtosecond laser-assisted pterygium surgery. The Z8 comes with two interfaces – liquid, and applanating, and crucially, the Z8’s interfaces have large numerical apertures. This gives far tighter Z-axis focusing, permitting lower power (in the nanojoule range) to be used, and this causes far less collateral damage than other femtosecond laser systems with smaller numerical apertures. This is particularly important in opaque and translucent media (like the conjunctiva) – and the fact that the Z8 can do this is what enables us to use it to perform FLAPS. Our aims were twofold: to assess the feasibility and the reproducibility of FLAPS using the Z8 in porcine eyes (Figure 3). We performed a two-surgeon study; one surgeon was me, an experienced femtosecond laser user, the other a novice. We made 10 grafts of varying diameters, at depths of 60 and 100 µm, and the outcomes measured included the speed of the laser dissection, and conjunctival autograft size and thickness.
The Z8 was able to create the grafts – and we were happy to learn that there was no significant difference between the size of the graft we programed and the size of the graft that was produced. The mean time to achieve a 60 µm graft was around 18 seconds, which rose slightly to just over 20 seconds for 100 µm grafts. Histological studies showed that the Z8 does not disrupt the vessels in the cornea, and that it achieved a very planar cut – in essence, the Z8 gives you the same level of cutting precision in the conjunctiva as it achieves in the cornea. Finally, the Z8 leveled the playing field between the experienced and the novice surgeon, with both achieving similar depth results. I was approximately three seconds faster than my fellow surgeon (novice femtosecond laser user) in creating the grafts, and the grafts we created were of similar depth too. Recently, we received IRB approval to perform FLAPS on patients. The first was a gentleman with a small pterygium with lots of recurring inflammation. I removed it in the usual manner and did a Tenon’s resection to give a nice bare scleral bed. Once the bed was harvested, I marked the conjunctiva, rotated the eye down and applied the laser interface on top, and the Z8 took 35 seconds to do the cutting. I’d set the laser to create a 65 µm cut; once placed on the cornea, intraoperative OCT measured it at 67 µm. The conjunctival graft came off easily. The graft was stuck with fibrin glue and transferred over the sclera defect. I compressed the edges (as per normal conjunctival surgery), completing the placement of the graft. Hearteningly, we saw complete epithelial closure on the surface of the site where the graft had been harvested from after only eight days, and at one month post-op, OCT angiography showed that the graft’s blood vessels had been canalized with new vessels from the conjunctiva. So with the Z8 you truly have one femtosecond laser platform that can perform corneal, presbyopia, cataract, and now pterygium, surgery.
References
- KD Neff et al., “Comparison of central corneal graft thickness to visual acuity outcomes in endothelial keratoplasty”, Cornea, 30, 388–391 (2011). PMID: 21045647.
