
Dr. Faktorovich
Epithelial integrity is essential to producing favorable patient outcomes for both corneal and lens refractive surgery. With LASIK, in particular, the epithelial loosening that occurs during a flap lift in patients with epithelial basement membrane dystrophy (EBMD) can cause delayed healing and reduced visual acuity on postoperative day one, preventing the patient from experiencing the “LASIK miracle” of 20/15 – or even 20/10 – uncorrected vision.
A patient’s history of recurrent erosions, as well as corneal findings at the slit lamp, are the mainstays of diagnosing EBMD. When EBMD is diagnosed, the best refractive procedure for the patient is often photorefractive keratectomy (PRK), rather than LASIK or lens-based surgery. However, some patients with subclinical EBMD don’t manifest any signs or symptoms, and so the first sign of the condition can be the unexpected epithelial loosening during LASIK flap lift. In such cases, epithelial thickness mapping (ETM) using widefield OCT might help to screen patients pre-surgery, to detect subclinical and subtle EBMD, helping the surgeon determine the best procedure for the patient.
In patients with normal corneas, epithelium is a few microns thicker inferiorly versus superiorly (1), and it is thicker nasally versus temporally (2). Our analysis of ETM patterns in 317 myopic eyes with normal corneas showed inferior epithelium to be 3.05+/-0.05 microns thicker than superior epithelium. Additionally, we analyzed ETM patterns in 10 patients with mild/subclinical EBMD. Five patients were asymptomatic and with clear corneas preoperatively. They underwent LASIK, but their epithelium loosened during flap lift. Another five patients had mild signs of EBMD. Two patients had a history of recurrent erosions, but their corneas were clear. Three other patients had few mild findings on the slit lamp exam – one patient had a single small micro cyst in the periphery, another had a small area of negative staining, and another patient had a small area of fingerprint pattern on the cornea. These five patients with mild signs and symptoms underwent PRK. Preoperatively, all patients were screened with topography, tomography, and ETM with widefield OCT.
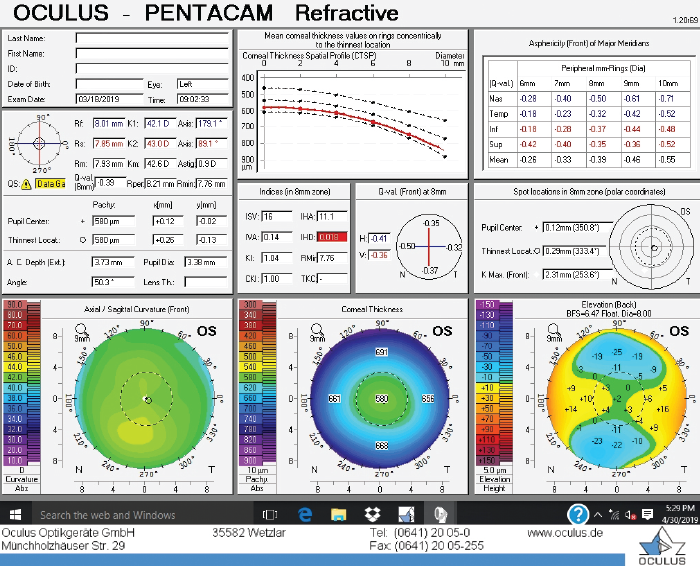
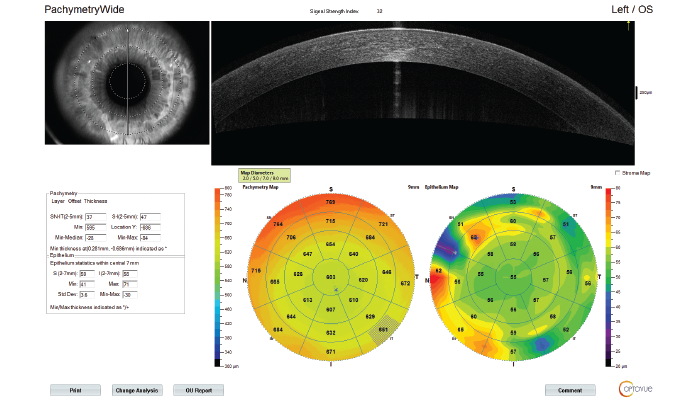
Two out of the 10 patients had normal ETM; the other eight patients’ ETMs were abnormal. Two had inferior epithelial thickening, corresponding to the area of inferior steepening on topography. In these instances, we have found ETM to be a helpful tool in determining whether inferior topographic steepening is due to potential keratoconus versus EBMD. In patients with keratoconus and even forme fruste keratoconus (FFK), inferior topographic steepening may correlate with epithelial thinning on ETM (see Figure 1A and 1B), and so keratorefractive surgery may need to be avoided in these patients.
In patients with EBMD, inferior topographic steepening may correlate with epithelial thickening on ETM (see Figure 1C and 1D); these patients can respond positively to PRK.
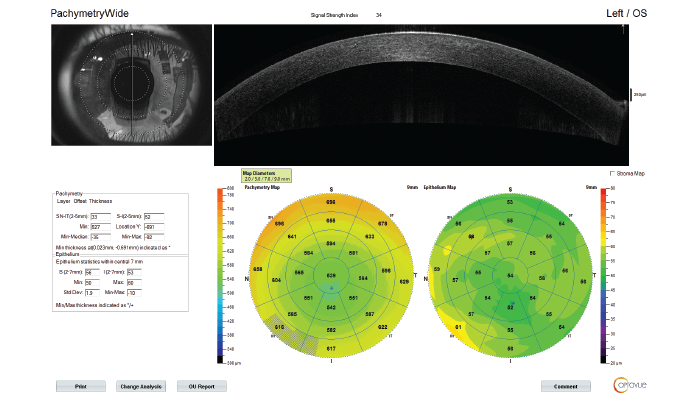
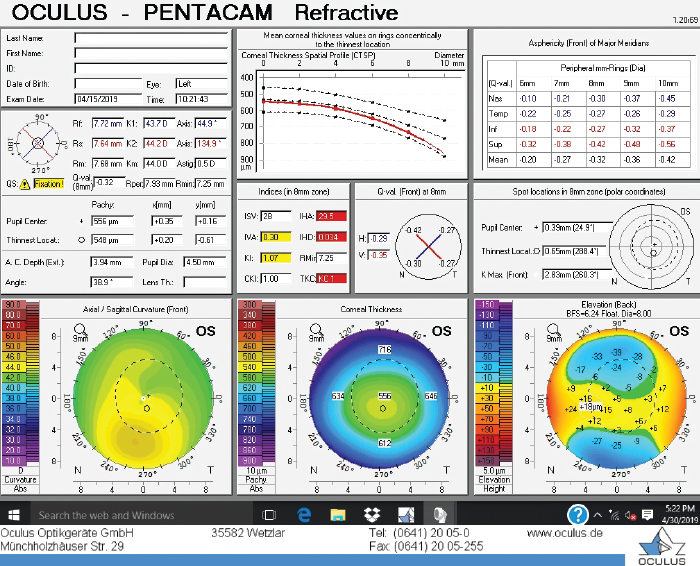
ETM in patients with inferior corneal steepening due to keratoconus (A,B) vs. EBMD (C,D) Epithelium is thinner in the area of inferior corneal steepening in patient with keratoconus and thicker in patient with EBMD
Another two patients had focal epithelial thickening corresponding with the location of elevation on topography superiorly, nasally or temporally. The areas of topographic elevation with corresponding areas of epithelial thickening on ETM were typically bilateral.
Four other patients had a peripheral ring of alternating areas of epithelial thickening and thinning. In one patient, corneal exam was initially recorded as normal, but a subsequent ETM revealed a peripheral ring of alternating thick and thin epithelium (see Figure 2A). The cornea was then re-examined and very subtle fingerprint lines were discovered in the periphery (see Figure 2B). In this patient the ETM helped to diagnose EBMD, and the patient was recommended for PRK rather than the LASIK surgery he was originally scheduled for.
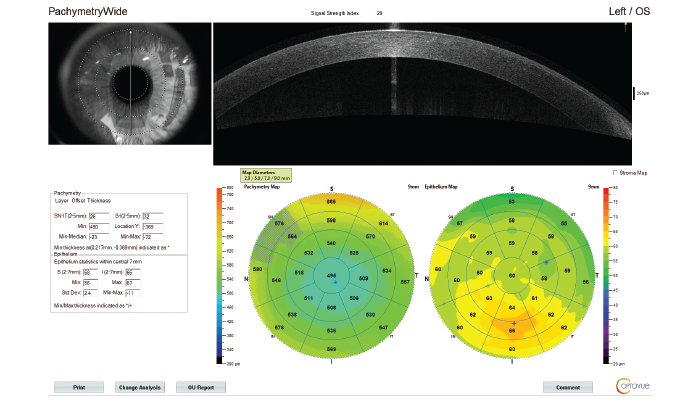
ETM in patients with inferior corneal steepening due to keratoconus (A,B) vs. EBMD (C,D) Epithelium is thinner in the area of inferior corneal steepening in patient with keratoconus and thicker in patient with EBMD
At the Pacific Vision Institute in San Francisco, we currently undertake ETM with widefield OCT to screen all patients coming in for refractive surgery evaluation. This method often helps to differentiate between different causes of inferior steepening, allowing us to recommend procedures appropriate for each patient. It also helps to diagnose EBMD in patients with minimal signs and symptoms, which again helps to avoid the unexpected epithelial loosening during flap lift.
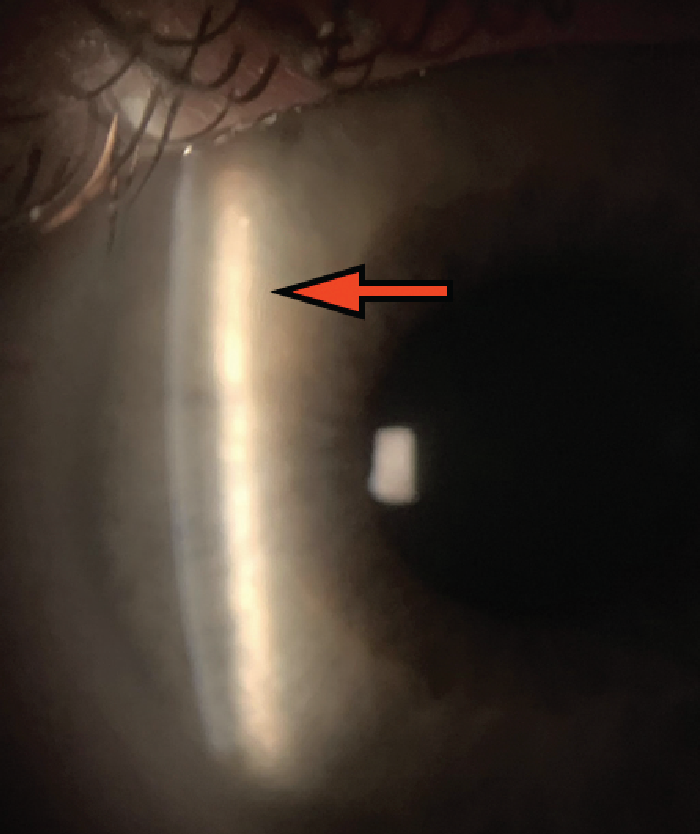
ETM (A) in patient with faint fingerprint lines on slit lamp corneal exam (B)
References
- DZ Reinstein et al., “Epithelial thickness mapping for corneal refractive surgery,” Curr Opin Ophthalmol, 33, 258 (2022). PMID: 35779050.
- N Pircher et al., “Distinguishing keratoconic eyes and healthy eyes using ultrahigh resolution optical coherence tomography-based Corneal Epithelial Thickness Mapping,” Am J Ophthalmol, 189, 47 (2018). PMID: 29458037.
