- The ICO-Allergan Advanced Research Fellowship was launched in 2017 to support young ophthalmologists in continuing their research
- Emilio de Almeida Torres-Netto, of the University of Zurich, Switzerland, is the inaugural recipient of the Fellowship
- Torres-Netto discusses his research into corneal biomechanics and keratoconus, and describes how he will continue his research in the coming year
- Nominations are now open for the 2019 ICO-Allergan Advanced Research Fellowship.
2018 marked the inaugural ICO-Allergan Advanced Research Fellowship – an award specifically designed to help young ophthalmologists continue their research (see Box - The ICO-Allergan Advanced Research Fellowship). The recipient? Emilio de Almeida Torres-Netto, a cornea, cataract and refractive surgery specialist currently at the University of Zurich, Switzerland. Hot on the heels of officially receiving his award at the World Ophthalmology Congress (WOC; 16–18 June, 2018; Barcelona, Spain), we spoke to Torres-Netto to hear about his research – and what he hopes to achieve over the coming year.
Finding satisfaction in a challenge
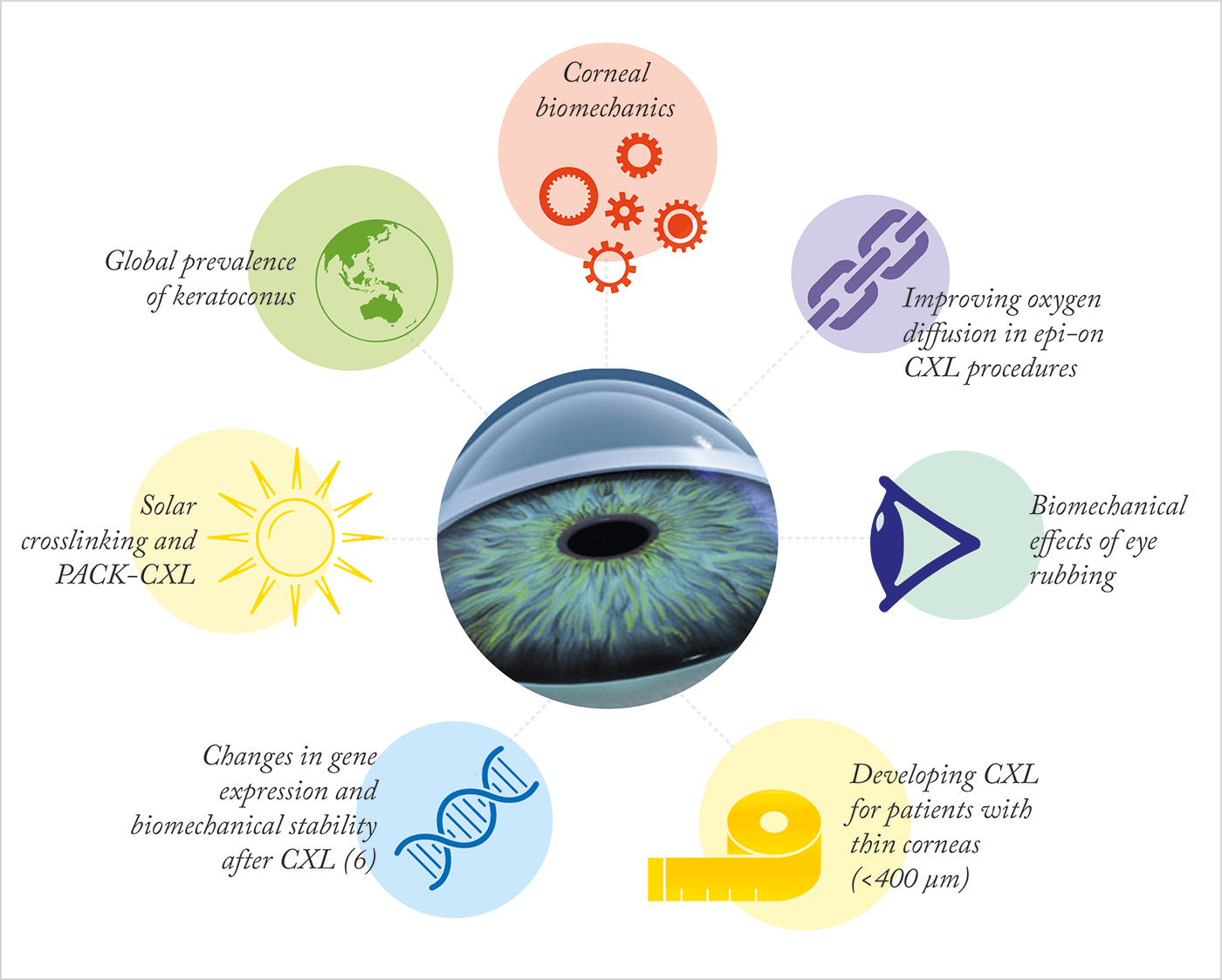
Although I completed three specialties – cornea, cataract and refractive surgery – I have always had a particular interest in keratoconus. Perhaps because it is a challenging disease to treat, and its prognosis has changed a great deal over the years. Previously, the only treatment available was penetrating keratoplasty, which dealt mostly with the most advanced cases. And although new modalities of treatments have been developed, including the global standard of corneal crosslinking with UV-A light and riboflavin, there is still room for further development. The new perspectives that are being pursued, and the possibility to research and further develop in this field, have inspired my interest in keratoconus. It is amazing to receive the ICO-Allergan Advanced Research Fellowship to help further my research in keratoconus and corneal crosslinking (CXL) with Farhad Hafezi at the University of Zurich, Switzerland (see Box – Next Steps in Keratoconus Research).Improving crosslinking
Treating progressive forms of keratoconus is one of our key areas of interest, and we are deeply involved in investigating how to make the crosslinking procedure more effective. As part of our work, we have been looking into how to improve the effectiveness of epi-on CXL assisted with iontophoresis (epi-on I-CXL). Epi-on techniques have so far produced unsatisfying results. Our group demonstrated that crosslinking doesn’t occur in the absence of oxygen (1), hence it is likely that stromal oxygen concentration might be too low when the epithelium is intact. Recently, we presented findings that proved we could significantly increase the biomechanical effect of epi-on I-CXL ex vivo when using a low irradiance (1.5 mW/cm2) and long irradiation time (60 minutes) – double the time of the Dresden protocol – indicating that oxygen diffusion may remain as a limiting factor (2). Although this epi-on I-CXL procedure is still less effective than epi-off CXL, our modified method might improve efficiency of the procedure and help establish this method as an alternative CXL treatment option; for instance, in special cases or low-compliance patients. Moreover, our preliminary laboratory studies have also shown that temperature might be an important factor for oxygen diffusion in the CXL procedures, and we are hoping to investigate if cooling the tissue using chilled BSS could increase oxygen diffusion deeper into the corneal stroma.It’s a mechanical thing
Improvement of current excimer and femtosecond laser technology is also part of our ongoing studies. In 2017, we showed how modulating excimer laser parameters could potentially decrease corneal inflammation (3). We are still working on modulating excimer laser parameters to try and diminish inflammation, as this could be useful in complex cases and have a central role in the haze formation pathway. Biomechanical impacts on the cornea are another area of interest in my research. In terms of keratoconus, we are hoping to investigate how eye rubbing might affect the biomechanical properties of the cornea. Although the keratoconus community agrees that eye rubbing is a major risk factor for progressing keratoconus, it has not yet been proven how the mechanics of eye rubbing directly affects biomechanical properties of the cornea. We have just developed a machine that can simulate eye rubbing and we are looking forward to the answers we can get from this project.What? The $50,000 Fellowship supports the continuation of innovative research that advances scientific understanding and clinical management of ophthalmic diseases worldwide. Who? Young ophthalmologists (below the age of 40), who have at least 12 months research training. When? Applications are now open for the 2019 fellowship, and the winner will be notified at ARVO 2019 annual meeting in Vancouver, Canada. How? Application instructions and more information can be found here.
Looking to the sky
UV light from the sun is often used in lower income regions to clean and sterilize water. As UV light is an integral part of the crosslinking procedure, we wondered if we could harness UV light from solar energy to perform ‘natural’ crosslinking. This could have a huge impact in regions and countries with lower incomes. We’re not yet sure exactly how to crosslink corneas using the sun, but we are currently working on a procedure involving oral riboflavin that does not require epithelial debridement. Developing a feasible, and most importantly effective, epi-on procedure would be fantastic – and we are hopeful! Furthermore, as resistance to antibiotics is a global problem that we will have to face in the coming decades, we are also working on enhancing photoactivated chromophore for infectious keratitis (PACK)-CXL to treat corneal infections. Such a treatment would be highly beneficial for low income regions and could benefit many patients, and we are currently working on multicenter clinical and laboratory studies to make this treatment a reality.Challenging dogma
The prevalence of keratoconus is commonly cited to be 0.05 percent (4), suggesting it to be a rare disease. Looking deeper into this statistic, it became clear that it arose from a 48-year study, from 1935 through 1982, based on limited technology: light retinoscopy and keratometry mires were used to examine patients. As we can detect and diagnose keratoconus with a greater accuracy than before, we must question if this number really is up to date. Recently published papers from different geographical regions suggest not. To test, we performed a pilot study in Saudi Arabia. Although some publications have already identified a higher prevalence of keratoconus in the Middle East, we identified a prevalence of 4.8 percent using Scheimpflug imaging – almost 100 times higher than the commonly cited 0.05 percent prevalence (5). It’s a huge difference and, because of this, establishing the global prevalence of keratoconus is one of our major projects at the moment, and we’re currently collecting data in several countries to establish the real prevalence of keratoconus based on modern diagnostic instruments.Moving on and up
Although these are the main projects that I’m working on (and those that the Fellowship will help support), we have much more going on! For example, our group also recently showed how genetic transcription occurs in response to CXL (6). It is an exciting time to be working in the field of keratoconus and corneal biomechanics, both clinically and in research, under the leadership of Farhad Hafezi. As keratoconus and corneal ectatic diseases are one of the most frequent causes of severe visual impairment in the young, we hope that this project will help strengthen our understanding of keratoconus and corneal biomechanics, and improve CXL technology to perform more effective and safer treatments. Emilio de Almeida Torres-Netto is currently completing a PhD and Research Fellowship at the Federal University of São Paulo, Brazil, in association with the University of Zurich, Switzerland.References
- O Richoz et al, “The biomechanical effect of corneal collagen cross-linking (CXL) with riboflavin and UV-A is oxygen dependent”, Transl Vis Sci Technol, 2,6 (2013). PMID: 24349884. EA Torres-Netto et al., “Oxygen diffusion limits the biomechanical effectiveness of iontophoresis-assisted transepithelial CXL”. Presentation at WOC – “Outstanding Paper Award”; 16–18 June, 2018; Barcelona, Spain. EA Torres-Netto et al, “Optimizing the inflammatory response after excimer laser ablation using molecular inflammatory markers”. ASCRS Best Paper of Session Winner; 5–9 May, 2017; Los Angeles, CA, USA. RH Kennedy et al., “A 48-year clinical and epidemiologic study of keratoconus”, Am J Ophthalmol, 15, 101 (1986). PMID: 3513592. EA Torres-Netto et al., “Prevalence of keratoconus in paediatric patients in Riyadh, Saudi Arabia”, Br J Ophthalmol, [Epub ahead of print] (2018). PMID: 29298777. S Kling et al., “Differential gene transcription of extracellular matrix components in response to in vivo corneal crosslinking (CXL) in rabbit corneas”, Transl Vis Sci Technol, 6, 8 (2017). PMID: 29242757.
