- Research institutes and eye banks must work closely together to secure a good pipeline of donor eyes and tissue
- All collaborating institutes need to recognize that organ harvesting and eye banking have significant costs – and fund accordingly
- Communicating clearly with potential donors and their families is the key to unlocking globe donation
- It’s vital to feed back to the donors’ families: let them know what their precious gift is doing to advance medicine and vision science
Remarkable advances in our understanding of the genetic and biological foundations of a number of major human ocular diseases have derived from studies of donated human eyes. As an example, early morphological and immunohistochemical studies of human eyes provided the first evidence that aberrant function of the complement system at the level of the RPE-choroid interface plays a key role in the etiology of age-related macular degeneration (AMD). Importantly, these studies led to the identification of an association of a common risk haplotype of the Complement Factor H (CFH) gene with AMD (1–4). According to a recent article in The Ophthalmologist, the number of eyes donated for research has declined over the last decade (5). But is it because (as was suggested) of fewer people being willing to donate their eyes? A recent study (6) confirmed that this was the case with some people, but apparently others would donate, but labor under the mistaken assumption that their eyes were “too old or unhealthy to be of any use.” The majority, however, simply hadn’t considered donating their eyes, because they hadn’t been made aware of the possibility.
Solutions to this problem are offered by Williams and colleagues (6), and include a recommendation that research institutions work more closely with eye banks. We agree with this concept wholeheartedly, but suggest that this alone is not enough to increase the availability of human eye tissue for research purposes. We believe there are a number of key ingredients that lead to successful and long-lasting partnerships, such as the one created here in Salt Lake City between the John A. Moran Eye Center (JMEC), the Sharon Eccles Steele Center for Translational Medicine (SCTM) and the Utah Lions Eye Bank (ULEB).
Our ingredients for success
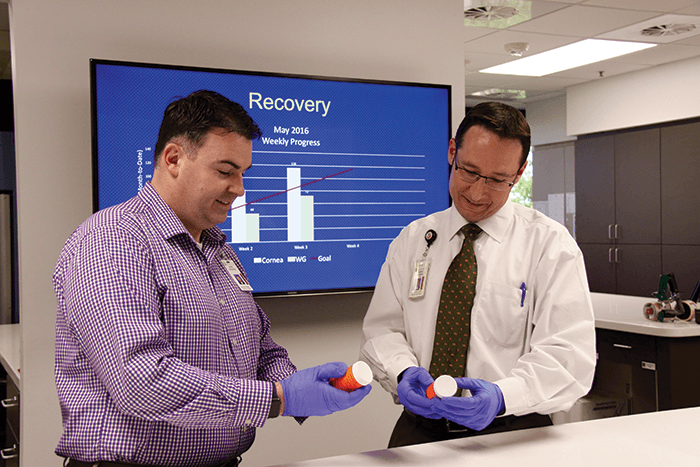
Communication has been the most important component of our successful partnership. At an operational level, it is critical that the overall need of tissue is established early in any partnership, as this dictates many of the partnership’s parameters. Once the need is established, we have learned that it is imperative that research institutions provide financial support to their eye bank partner. There are significant costs related to the acquisition of human eyes – and this is a fact that’s quite often unappreciated by investigators and their institutions. In our case, this cost includes having staff from both the ULEB and the JMEC/SCTM available at all hours, 365 days of the year, to ensure that we never have to turn down a donation of this very precious gift. The ULEB and JMEC/SCTM at the University of Utah have created one of the most productive research tissue placement systems in the United States. How? A decades-long partnership where money has been spent building and maintaining not only a robust tissue collection and processing program, but also supporting public outreach and education programs that center on eye donation. This last part is key. Together, we partner in educating potential donors, their families, caregivers, hospital staff members, local ophthalmologists and the general public about donation and the importance of ocular tissue to scientific discovery and the future of medicine. These educational activities are ongoing and are a critical component of this successful partnership. The JMEC/SCTM and ULEB use social media, community events and newsletters as platforms to educate and inform the public about the importance of tissue donation to research, often with Moran’s real-life research breakthroughs as examples.Keep the message simple
We have learned that simple messages – like “tissue can be used for research even if it’s not suitable for transplant” and “tissue derived from older individuals with and without eye disease are precious gifts” – are important to communicate. It’s here where our long-established partnership pays dividends: ULEB employees are exquisitely skilled in having delicate conversations with patients and their families, and Moran scientists and physicians call upon them regularly to help communicate donation options and needs. Feedback to donor families is equally important and both partners strive to ensure that this occurs – for example, SCTM staff members are in contact with the majority of donor families, often leading to the participation of the donor’s family members in other research studies.So far so good
The symbiotic arrangement between the ULEB and JMEC/SCTM has been wonderfully productive. The Moran Eye Center provides physical space and salary support, subsidizing ULEB’s efforts and helping them to expand (the ULEB recently built a new, state-of-the-art center with an increased capacity for receiving and processing tissue). In return, Moran scientists and clinicians have access to higher-quality, lower-cost tissue than they would from out-of-state eye banks. The ULEB provided 11,381 eyes to researchers between 2012 and 2015, and in 2015 was the fourth highest in terms of research tissue placed in the US. For SCTM, the ULEB has provided 3,401 fresh globes (i.e. tissue recovered within five hours) since 2010. The significance of fresh tissue is vitally important for Moran scientists and clinicians due to the fact that significant cell death occurs once blood circulation in the body ceases, meaning that it’s imperative that most tissue is provided within a short timeframe to enable scientists and researchers to glean the best, most accurate results from their experiments.The will is there!
We propose that the key issue at hand is not that “the number of people willing to donate their eyes for research purposes has been falling.” Our experiences have taught us that patients who are educated about tissue donation are willing to donate for both transplant and research; and that families are comforted that their loved one gave a lasting gift of sight, whether for today or for tomorrow. People are more than willing to donate their eyes! The challenge of increasing the availability of ocular tissue lies with the creation of robust partnerships, commitment of time and staff, active cooperation and communication, financial investment, promotion, education and, importantly, feedback to all who have participated in the donation and acquisition of these precious tissues. The eye donation program here in Utah has been a resounding success because of these key ingredients.Chris Hanna is the Executive Director of the Utah Lions Eye Bank and Gregory S. Hageman, is the John A. Moran Presidential Professor and Executive Director of the Sharon Eccles Steele Center for Translational Medicine at the University of Utah Moran Eye Center in Salt Lake City.
References
- GS Hageman et al., “A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration”, Proc Natl Acad Sci U S A, 102, 7227–7232 (2005). PMID: 15870199. AO Edwards et al., “Complement factor H polymorphism and age-related macular degeneration", Science, 308, 421–424 (2005). PMID: 15761121. JL Haines et al., “Complement factor H variant increases the risk of age-related macular degeneration”, Science, 308, 419–421 (2005). PMID: 15761120. RJ Klein et al., “Complement factor H polymorphism in age-related macular degeneration”, Science, 308, 385–389 (2005). PMID: 15761122. R McGuigan, “Bring Out Your Dead”, The Ophthalmologist, 27, 14–15 (2016). Available at: top.txp.to/issues/0216/205. AM Williams et al., “Increasing the availability and quality of donor eyes for research”, JAMA Ophthalmol, 134, 351–352 (2016). PMID: 26768017.
