- ‘Top hat’ beam profiles illuminate the center of the cornea but for many patients with keratectasia, that is not the weakest part.
- Away from the center of the cornea, the top hat CXL effect drops off quickly.
- We have optimized the beam profile in second-generation CXL illumination devices.
- CXL should be carried out in every patient with keratoconus, and optimized beam profiles deliver a greater chance of success.
In keratoconus, the cornea is thinnest at the center and thickens towards the periphery, which yields the characteristic conical shape. As the thickness varies by both location and severity of disease, the thickness distribution of the cornea should be assessed before corneal collagen cross-linking (CXL) is undertaken. Our research at the Institute for Refractive and Ophthalmic Surgery (IROC) in Zurich, Switzerland, has shown that maximal corneal stiffness is achieved by centering treatment on the thinnest point of the cornea. In the majority of keratectasia cases, the thinnest point is typically 1 to 3 mm off the center of the cornea. We examined 22 eyes of patients with keratoconus, finding that the distance between thinnest point and the apex was between 0.2 to 1.2 mm apart. When we examined 38 eyes of patients with pellucid marginal degeneration, the distance ranged from 0.5 to 2 mm. These results strongly suggested that the apex should not be used as the reference point in either of these diseases, and that CXL treatment should be centered on the thinnest point, as identified by corneal tomography.
Standard beam profile
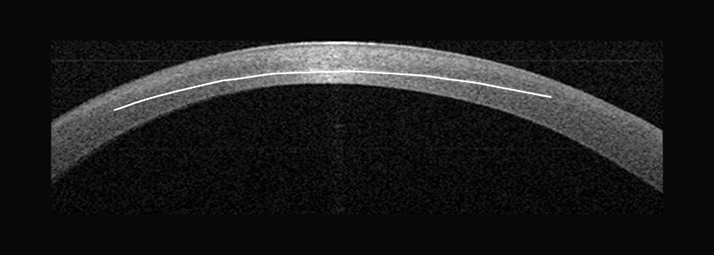
Historically, standard procedure has been to perform CXL with a ‘top hat’ beam profile, which involves constant illumination of the cornea, centering the illumination at the middle of the corneal apex. However, moving away from center of the beam the treatment effect rapidly becomes less effective. If the weakest point isn’t at the center of the apex, the clinical effect of CXL is significantly diminished (Figure 1). Consequently, we needed to rethink our approach, and to apply light specifically at the weakest area of the cornea.To confirm this requirement, we evaluated ten eyes with keratoconus using optical coherence tomography (OCT), one month after CXL was performed. We observed a lack of homogeneity of the beam in some of the older devices (UV-X1000, IROC, Zürich, Switzerland), however, the measured light distribution could only partially explain the reduced effect. The finding was associated with differential amounts of cross-linking at the center compared with the periphery of the cornea – indeed, corneal cross-linking was 25 percent lower in the periphery than at the center (1). This demonstrated that ‘top hat’ illumination is an unsatisfactory approach for generating homogeneous cross-linking throughout the cornea – particularly in the periphery. Simply put, the intensity of illumination needs to be increased as the beam moves away from the apical center, in order to achieve the required increases in cross-linking in those areas.
Optimized beam profile
Our working hypothesis was that increasing the light intensity in the periphery – over the thinnest point – will improve the outcomes of patients with keratectasia. To achieve this, we needed an improved, optimized beam profile (3). Using the IROC UV-X2000 system (IROC Innocross AG, Zug, Switzerland), we achieved 25−30 percent more cross-linking when using this new beam profile, as compared with other illumination systems (see Case Report). Examination of the demarcation line with OCT revealed that we had successfully produced a homogenous, thick layer of cross-linking across the entirety of the treated cornea (Figure 2).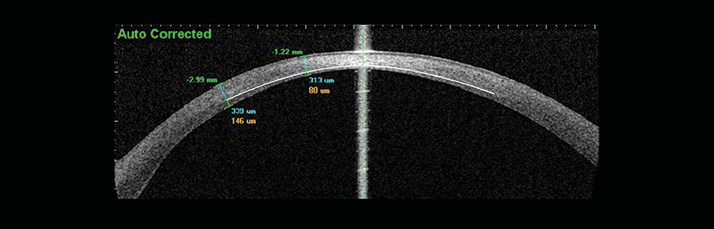
The original Dresden CXL protocol utilized a UV-light intensity of 3 mW/cm2 for 30 minutes. We evaluated a range of irradiance powers, from 3 to 90 mW/cm2, and found that 9 mW/cm2 produced optimal CXL (4), a result confirmed by other recently-published studies (5). This increased intensity has now been incorporated in the optimized beam profile, in addition to increasing the irradiance energy in the periphery (which has been raised by up to 7.2J/cm2). A useful side-benefit of the increased intensity is that the treatment duration is reduced to 10 minutes. Theo Seiler’s research group in Zurich has been investigating the effectiveness of optimized beam profile CXL with the IROC UV-X2000 system for the past two years (2). To date, thirty-eight eyes with regular keratoconus, no scars, and no previous surgery have been treated. All patients satisfied standard indications for treatment (namely, progression of greater than 1 diopter [D], age 35 years or less, and best spectacle-corrected visual acuity [BSCVA] less than 20/25), and thirty-six patients have completed the 12-month follow-up visit. All patients showed flattening of the cornea, with greater than 95 percent and greater than 65 percent showing flattening of 1 D and 2 D, respectively. These results are superior to those obtained with standard CXL, and importantly, a homogenous cross-linking depth across all eyes was observed, with similar effects in the periphery and the center. Complications were noted, but these were similar to those seen with standard CXL protocols. Second generation cross-linking devices require an optimized beam profile for best results. Although other reports have discussed optimized beam profile systems to reduce the treatment time, our research has focused on improving the effectiveness of CXL, and with it, the benefit to patients. Based on the data currently available, we believe that CXL – with an optimized beam profile – should be carried out in every patient with keratoconus.
Michael Mrochen is the Founder and CEO of IROC Science to Innovation, and co-founder of both IROC Innocross and Clearsight Innovations Ltd.
Case Report
As an example from our study, we present a 23-year old male, with documented keratoconus progression (steepening of more than 3 D within one year), which resulted in thin cornea (400 µm) and a BSCVA of 0.25 (20/80). At one month following the procedure, we observed homogenous cross-linking with a deep demarcation line. At 12 months, we observed substantial flattening of the cornea (>6 D) (Figure 3), resulting in a BSCVA of 0.7 (20/30).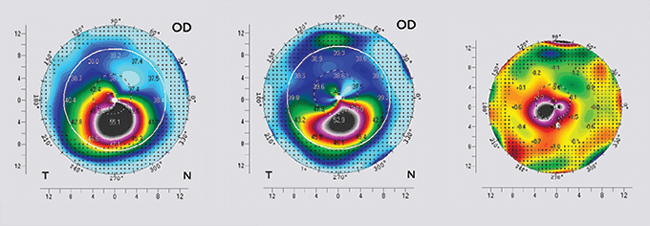
References
- T. Koller, S. Schumacher, F. Fankhauser II, T. Seiler, “Riboflavin/ultraviolet a crosslinking of the paracentral cornea”, Cornea, 32, 165–168 (2013). doi: 10.1097/ICO.0b013e318269059b.
