- Baby boomers are reaching old age
- They are causing a sharp spike in the number of cases of certain eye diseases
- Current therapeutic strategies are inadequate, especially if early signs of disease are missed
- The burden on ophthalmology services will be severe
- Strategies to address this impending disaster are urgently required
In the year 2000, there were 69 million people aged over 80 years in the world, according to United Nations data (1). By 2050, it is estimated that this number will have grown to 379 million, a more than fivefold increase. In Western countries, this increase is accounted for by “baby boomers”, the generation born between the mid-1940s and mid-1960s – essentially the spike in births following World War II. Baby boomers constitute a demographic timebomb, one that’s close to detonation: an unprecedented level of age-related disease will occur over the next three decades or so. This article examines the impacts that aging baby boomers will have on the practice of ophthalmology.
Boomers in sickness and health
Earlier in their lives, baby boomers were, according to Wikipedia, “the wealthiest, most active, and most physically fit generation up to that time, and amongst the first to grow up genuinely expecting the world to improve with time. They were also the generation that received peak levels of income, therefore they could reap the benefits of abundant levels of food, apparel, retirement programs, and sometimes even ‘midlife crisis’ products.” Today, the boomers refuse to accept that they’re getting old (Figure 1). The phrase “forty is the new thirty” became popular when they hit their fourth decade and their current mantra is “seventy is the new fifty”. In some respects, this is absolutely true. The lives of baby boomers have been far easier than those of their forebears: for them, physical exertion became a leisure activity or an occasional chore in order to keep fit rather than a way of life, and if certain parts of the body did wear out, replacements were available. Widespread vaccination during infancy shut out the ravages of diphtheria, tetanus, whooping cough and polio, and boomers have benefited from antibiotic therapy throughout their lives, mostly avoiding infection-related morbidity and mortality.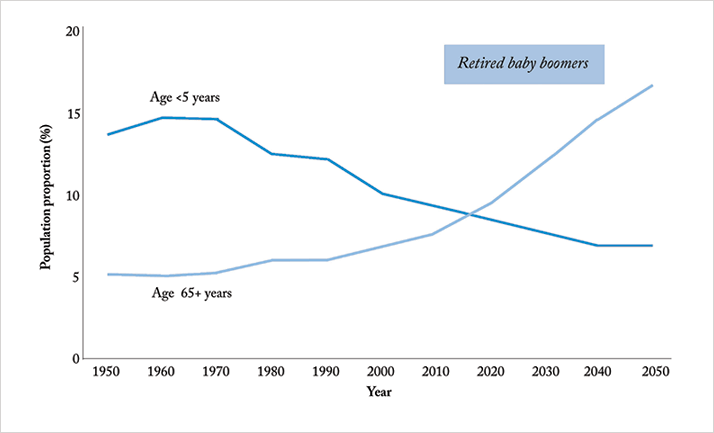
The eye, in some respects, is a success story too. There has been a rush to refractive surgery as tens of millions each year across the world choose to have laser vision corrective surgery; clear lens exchange is a huge market, and there are a number of presbyopia-correcting interventions with sales projections that are in the stratosphere (As a rule, these are to avoid wearing spectacles, something that in baby boomers’ minds is associated with old age). In most cases, the refractive outcomes in patients with premium IOLs is spectacular: a cloudy lens is removed and replaced with a clear lens that can also correct for astigmatism. Look beyond or, more accurately, behind the lens and the situation is far less positive. Ocular diseases of senescence gradually robbed the baby boomers’ parents of their sight and most of those diseases are still with us. That these conditions can’t be so easily kicked down the road or cured should alarm not just baby boomers but their children and their children’s children. Even with the best standard of care, the therapeutic options that work for these posterior segment diseases are not effective indefinitely. At the moment, it seems inevitable that a large proportion of baby boomers will end up with visual impairment – and the societal burden will skyrocket as their visual impairment progresses.
This article assess just how bad the situation is, and looks at the chances of medical science coming up with effective therapeutic interventions in time to avoid large-scale strife. The four eye diseases that present the biggest challenges to the baby boomer generation, namely age-related macular degeneration (AMD), diabetes-related eye disease, cataracts and glaucoma are addressed in turn.
Age-related macular degeneration
AMD is the leading cause of blindness in developed countries, and the third-leading cause in developing countries. Globally, between 20 and 25 million people are affected by AMD, and the World Health Organization (WHO) estimates that eight million people have severe blindness as a direct result of the disease (1). It is projected that the number of people with some form of AMD will double between now and 2050 (1). Tools to treat AMD are limited. Wet AMD is addressed reasonably effectively with anti-VEGF therapy, lasers and even low-voltage x-ray therapy, but it accounts for only 10 percent of all AMD cases. Very little can be done to treat the 90 percent of patients with dry AMD, beyond a recommendation to take high doses of vitamin supplements and antioxidants (2). Risk factors for the development of AMD have been identified, raising the possibility of avoiding the disease. Unfortunately, however, many of the factors aren’t modifiable. One, advanced age, clearly comes to us all. Hereditary elements represent some of the greatest risk factors (3). Numerous gene mutations and deletions have been described (4), but the interplay of genes in building an eye is majestic in its scale and there are the complexities of gene silencing and post-transcriptional modifications to contend with, even before any protein has been made. Replacing a gene (or genes) in early life may help (or may not) but it holds little hope for our baby boomers as it seems highly unlikely that simply adding a single gene to their senescent cells in the macula will induce retinal rejuvenation or vision improvement. However, the substantial amount of research on the topic may provide promising leads for tackling the genetic susceptibility to AMD.There are some modifiable risk factors, including smoking, hypertension, obesity, cholesterol, fat intake and oxidative stress (3) – an unfortunate cocktail of comorbidities that baby boomers present with all too regularly. Interventions here, should they work, would be highly effective and cost-effective. Smoking, hypertension and obesity are massive epidemics in in their own rights, and have been targeted by other medical specialties with countless interventions and initiatives, without overwhelming success. Hypertension and cholesterol are well managed by drugs – but this has been the case for decades, and AMD levels are still inexorably rising. For the other risk factors, new approaches to addiction and dietary management would be most welcome. The practical implications of the rise in AMD patient numbers are being felt everywhere. Retina clinics are massively oversubscribed, with specialists often working far longer than their allotted hours to get through the case loads, in part because intravitreal ranibizumab or aflibercept injections are time-consuming, and in many cases, need to be administered monthly. Improved ways of treating wet AMD that involves fewer clinic visits are needed, whereas novel approaches for dry AMD are a desperate requirement.
Diabetes-related eye disease
The demographics of diabetes are profoundly worrying. The prevalence for all age-groups worldwide was estimated to be 2.8 percent in 2000 and is projected to reach 4.4 percent by 2030 (5). The elderly are affected disproportionately in these projections, with the hardest hit group of all being the baby boomers (see Figure 2).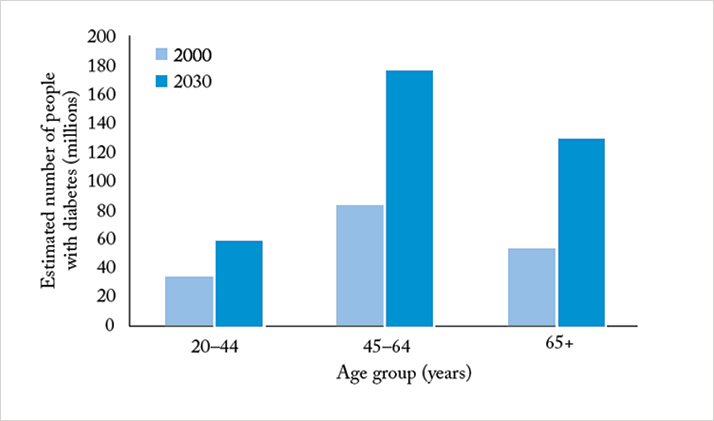
Diabetes doubles a person’s risk of glaucoma and it is also a major risk factor for corneal problems, cataract and macular edema (6–8). Furthermore, approximately two-thirds of people with diabetes have some form of diabetic keratopathy, which can include recurrent erosions, ulcers, corneal edema, and delays in wound healing (6–9). Of patients that do develop a keratopathy, those with diabetes are likely to experience a more severe form, respond to treatment less well, and recover more slowly (6). Glucose is the fuel that drives all cellular respiration. It is a highly reactive aldehyde and some of the by-products of its reactions can damage cells. For short-lived cells that are routinely replaced that’s okay, as they’re not around long enough for significant damage to occur. But in long-lived cells like neural (and retinal) tissues and in stable protein structures like the crystallins in the lens and the cornea, it causes cumulative deterioration. Tissues exposed high levels of glucose, such as the vasculature and the pancreas also sustain damage. Indeed, the root cause of the retinal and choroidal damage in diabetes is this vascular and local tissue damage, resulting in inflammation.
The effectiveness of current therapeutic interventions is variable. Cataract and glaucoma are dealt with separately below. Diabetic keratopathies are treated in the same manner as any other keratopathy from a non-diabetic origin, with topical therapies, scraping or laser therapy, or corneal transplantation, as appropriate. The issue with the last of these interventions is that there is a shortage of corneas to transplant today: it seems highly unlikely enough will be donated for transplantation in 2030 to cope with the demand. For DME, treatment with lasers, anti-VEGF therapies, or long-acting steroid implants can be effective. Just like their use in wet AMD, anti-VEGF drugs tend to be administered monthly in order to inhibit the macular neovascularization that results in the swelling and distortion of the macula. But again, this requires monthly visits of patients to ophthalmology clinics and that is something that’s not going to be sustainable. If anti-VEGF therapy fails, the next line of treatment looks like being intravitreally-implanted steroids. The steroids act to reduce the macular swelling, and they are now available in slow-release formulations that allow therapeutic doses to be administered for as long as three years, obviating the need for monthly intravitreal anti-VEGF injections. On the other hand, the use of steroids raises risks other adverse events, primarily cataracts. These can be dealt with, but as we’ll see in the next section, those that do develop cataracts will have to join the queue for treatment.
Cataract
Despite the earlier paean to the outcomes with cataract surgery, the fact remains that cataracts present a massive and worsening healthcare and societal problem. Of the 39 billion people today that are blind, almost 18 million are so because of cataracts, with the burden disproportionately affecting developing countries. Will the burden overwhelm the capacity to cope? It’s certainly a concern. Delaying the onset of cataract formation by a decade (or by otherwise avoiding the associated vision loss) could almost halve the demand for cataract surgery (10,11). In the absence of any pharmaceutical cataract prophylactics, the possibility of adjusting risk factors has taken center stage. Age plays a role, as do genetic factors (particularly in pediatric cases), but these are essentially unmodifiable. Radiation is a better proposition. X-ray, microwave and ultraviolet (UV) light exposure – particularly UV-B radiation – have been shown to cause cataracts (12–15). UV-B exposure can be sharply reduced easily and cheaply with sunglasses, and evidence exists that wearing sunglasses from an early age protects against cataract formation. However, ask any parent how difficult it is to make children wear sunglasses for extended periods on sunny days…Smoking is a risk factor, calling attention once more to the challenges of delivering effective public health interventions; it is incredibly difficult to get smokers to kick the habit.If lifestyle modification can’t be implemented, what alternative methods are there for delaying cataract formation? For a while, it seemed that antioxidant dietary supplements might delay or prevent cataract formation, but this proved not to be the case after bigger and better evaluations. So, short of a drug that protects the crystallin in the lens from becoming opaque (or replacing the crystallin with a functional and transparent equivalent), it would appear that an awful lot of baby boomers will be lining up for cataract surgery. Clinics must set up to cope with this influx of patients. Increasing patient throughput can help, although it is notable that femtosecond lasers procedures currently take longer than manual capsulorhexis. One likely measure is that as many delegable responsibilities as possible will be performed by support staff, leaving the ophthalmologist to perform procedures in a robot-like, production-line manner. The stark alternative is a society filling with aging, visually impaired, and therefore profoundly disabled, people; people who have a treatable condition but must wait for years and years to be seen.
Glaucoma
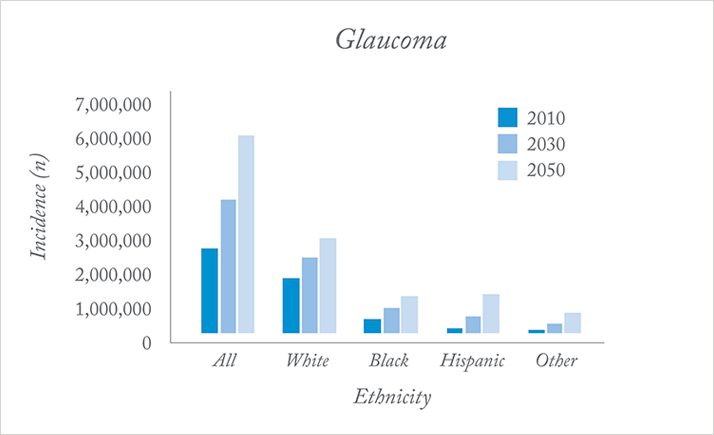
According to the WHO, 60.5 million people across the globe suffer from glaucoma, with 1–2 percent of the world’s population developing the diseases every year (16). Of the 60.5 million with glaucoma today, 8.4 million are blind. Most common is open-angle glaucoma, which afflicts 45 million people, 10 percent of whom are blind. However, in 2020 the total is projected to hit 80 million (16), most of whom will be baby boomers. For such a pernicious, age-related disease, the future for baby boomers with glaucoma is not as gloomy as it sounds – as long as screening picks it up (Figure 3). In the UK, according to the International Glaucoma Association, all but 5 percent of patients with an early diagnosis of glaucoma retain useful sight for the remainder of their lives. This functional vision, as opposed to blindness, is incredibly valuable: it enables people with glaucoma to continue to function independently, and not being blind has huge societal and economic benefits. For patients diagnosed with advanced-stage glaucoma it’s the opposite story: blindness is staved off for a short period, but functional blindness is not far away.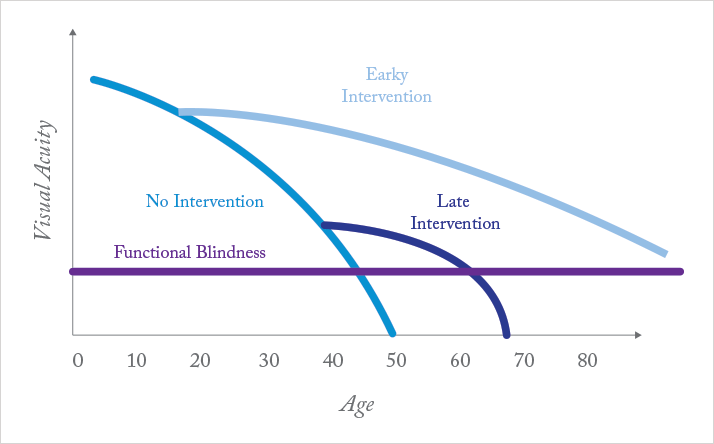
Making an early diagnosis is not easy, since; in glaucoma, sight loss is slow and gradual. Most cases of primary open-angle glaucoma are symptomatic only when significant vision loss has occurred (17). The pathogenesis is complex, involving multiple concurrent processes besides raised intraocular pressure (IOP). These include retinal pigment epithelial cell death, optic nerve damage, neurodegeneration that progressses into the brain, and even damage to anterior segment structures. Some presentations of glaucoma lack even elevated IOP (17).
The ocular changes can be observed by a combination of fundoscopy and optical coherence tomography (OCT) imaging, suggesting that these procedures should be added to tonometry for routine glaucoma screening (18). That’s the good news; the bad news is that the overwhelmed healthcare systems of the future may be unable to devote the time and budget required to perform glaucoma screening. Thus, what is currently a highly treatable condition (with topical eyedrops or surgical intervention) that has good outcomes if caught early enough may insidiously become more severe. It may even rob an increasing number of people of their sight for decades to come. This disease lacks modifiable risk factors that can be attacked (19). The one possibility is that people with glaucoma are more likely to have hypertension, and blood pressure can be controlled with a variety of well-established medications. Trauma and other ocular diseases can also result in glaucoma, but these are almost impossible to mitigate against, and the remaining risk factors are genetic and ethnic (Figure 4). For the foreseeable future, the best hope for glaucoma control is early, effective screening.
Can this bomb be defused?
The sheer number of baby boomer patients is already remarkable; they have stretched the ophthalmology infrastructure to its limit. And that patient number is not yet close to peaking. At the least, a large number of boomers will receive sub-optimal treatment; at worst, the system will suffer catastrophic failure. Improving the infrastructure is absolutely essential. Yet ophthalmologists will be in scarce supply. Currently, the numbers joining and leaving the profession are in balance, while the projected patient numbers demand a linear growth in the number. Given the many years of medical then postgraduate training that is required to create a new ophthalmologist, there seems to be no obvious solution to this part of the problem. Other areas of medicine are facing their own baby-boomer issues, suggesting that competition for physicians will be increasingly fierce.What’s certain is that the job of an ophthalmologist in ten or twenty years’ time – or even in five years’ time – will not look remotely like it does today. Any suggestion of inefficiency will have been removed and everything that can be delegated to support staff will have to be. Routine procedures will become even more production line-like than they are currently and face time with patients will be at a premium, something that is not conducive to best patient outcomes. There will of course be positive developments that will help the field to cope, and perhaps even to thrive. Undoubtedly, effective new surgical interventions will be developed, and many new small-molecule drugs and biologics will be introduced. This is unarguably the most exciting and fast-paced period for both scientific progress and the development of new ophthalmology practice.
Big data will also play a role. The data-mining of entire nations’ medical records may be controversial in terms of privacy, but it will help identify patients at risk of developing diseases like glaucoma, and it can automatically prompt these patients to go for a check-up. This in itself will save the sight of hundreds of thousands of baby boomers with glaucoma in the next decade. In perhaps two decades from now it will be possible do incredible things with stems cells, including rebuilding tissues in vitro for subsequent surgical implantation, or spraying stem cells onto the retina to replace and repair diseased cells.
Retinal implants will be a mature technology in the not-too-distant future, and the daily advances being made in the meantime mean that they will soon be easier to implant and give better vision than they do today. However these are complex surgical interventions and may be destined only for the privileged few. It is impossible to say where biomedical science will take us. Basic research continues to identify and characterize therapeutic targets, and many compounds that have the potential to treat currently untreatable diseases like dry AMD have been identified. A slew of new drug candidate molecules for ophthalmic diseases are being screened and evaluated right now. There is definitely hope. In the meantime, there is much to do at the population level to reduce the risk of patients developing cataracts, diabetes, macular degeneration, and to be vigilant for glaucoma. Baby boomers deserve no less.
References
- A. Chopdar, U. Chakravarthy, D. Verma, “Age Related Macular Degeneration”, BMJ, 326, 485–488 (2003). J.S. Tan et al., “Dietary antioxidants and the long-term incidence of age-related macular degeneration: the Blue Mountain Eye Study”, Ophthalmology, 115, 334–341 (2007). doi:10.1016/j.ophtha.2007.03.083. Age-Related Eye Disease Study Research Group. “Risk factors associated with age-related macular degeneration. A case-control study in the age-related eye disease study: Age-Related Eye Disease Study Report Number 3”, Ophthalmology, 107, 2224–2232 (2000). G. Hageman, “To Cure AMD, First Define It”, The Ophthalmologist, 2, 14–20 (2013). S. Wild, “Global prevalence of diabetes: estimates for the year 2000 and projections for 2030”, Diabetes Care, 27, 1047–1053 (2004). doi: 10.2337/diacare.27.5.1047. K. Skarbez et al., “Comprehensive Review of the Effects of Diabetes on Ocular Health”, Expert Rev. Ophthalmol., 5, 557–577 (2010). National Eye Institute, “Facts about Diabetic Retinopathy”, http://www.nei.nih.gov/health/diabetic/retinopathy.asp, Accessed February 26, 2014. V.S. Jeganathan, J.J. Wang and T.Y. Wong, “Ocular associations of diabetes other than diabetic retinopathy”, Diabetes Care, 31, 1905–1912 (2008). doi: 10.2337/dc08-0342. R.O. Schultz et al. “Diabetic keratopathy”, Trans. Am. Ophthal. Soc. 79, 180–199 (1981). A. Taylor, “Cataract: relationship between nutrition and oxidation”, J Am Coll Nutr., 12, 138–146 (1993). B. Garry, T. Hugh, “Cataract blindness: challenges for the 21st century”, Bull. World Health Organ. 79, 249–256 (2001). doi:10.1590/S0042-96862001000300015. S. Wang, J.J. Wang, T.Y. Wong, “Alcohol and eye diseases”, Surv. Ophthalmol., 53, 512–525 (2008). doi:10.1016/j.survophthal.2008.06.003. J. van den Brûle, F. Degueldre, A. Galand, “Drug-induced cataracts”, Rev. Med. Liege., 53, 766–769 (1998). D.H. Sliney, “UV radiation ocular exposure dosimetry”, Doc. Ophthalmol., 88, 243–54 (1995). R.M. Lipman et al., “Cataracts induced by microwave and ionizing radiation”, Surv. Ophthalmol., 33, 200–210 (1988). A. Cook, P Foster, “Epidemiology of glaucoma: what’s new?”, Can. J. Ophthalmol., 47, 223–226 (2012). doi: 10.1016/j.jcjo.2012.02.003. E.E. Chang, J.L. Goldberg, “Glaucoma 2.0: Neuroprotection, Neuroregeneration, Neuroenhancement”, Ophthalmology, 119, 979-986 (2012). T.C. Chen, “Spectral domain optical coherence tomography in glaucoma: qualitative and quantitative analysis of the optic nerve head and retinal nerve fiber layer (an AOS thesis)”, Trans Am Ophthalmol Soc., 107, 254–281 (2009). J.M. Seddon, “Genetic and environmental underpinnings to age-related ocular diseases”, Invest Ophthalmol Vis Sci., 54, 28–30 (2013). doi:10.1167/iovs.13-13234.
