- For the typical patient, RLE does not satisfactorily resolve dysfunctional lens syndrome, and may cause more problems than it cures
- Many implanted lenses cause significant forward light scatter, and none improve presbyope accommodation
- Over time, lens implantation increases the risk of photic phenomena, retinal detachment, lens dislocation and visual impairment
- It is time to rethink the rationale behind RLE – and re-evaluate whether it is as safe and effective as people think.
Refractive lens exchange (RLE) is becoming an increasingly common procedure. Typically, people in their early 40s and 50s, who have disposable funds, elect for the operation to address deteriorating vision or gain spectacle independence. In the short term, they appear happy with the procedure; RLE seems to gives them what they want (1). But is patient satisfaction with early postoperative outcomes lulling us into a false sense of security? Some ophthalmologists are starting to question whether RLE is as safe – and effective – as we think. Indeed, in my practice, I now try to talk patients out of it. Why? Because I believe that, for the typical RLE patient, the procedure risks adverse outcomes for little or no long-term benefit. Let’s look at the evidence.
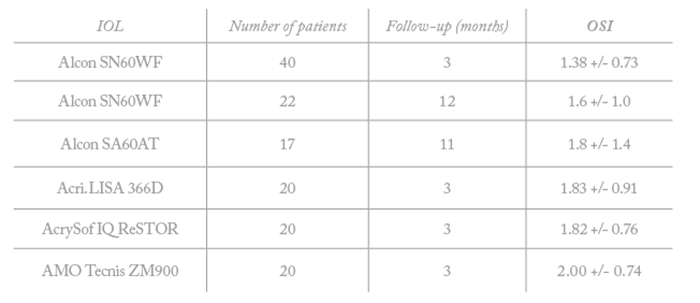
It’s useful to consider what visual problems RLE patients seek to resolve, and to what extent current IOLs actually address those problems. Briefly, patients request RLE because they have one or more symptoms of dysfunctional lens syndrome (DLS) – presbyopia, disability glare, decreased contrast sensitivity and decreased night-time vision. DLS symptoms such as disability glare are caused by forward light scatter from an early cataract; it’s been said that if the ocular scatter index (OSI) value is greater than one, then you should consider surgical intervention (2). The assumption is that providing an IOL will improve their DLS symptoms – but I believe this deserves to be examined more closely.
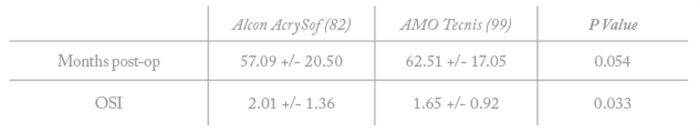
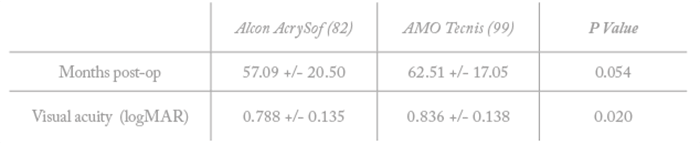
My first concern is that the majority of current IOLs actually produce forward light scatter (Table 1) – so they may end up causing the very problems patients hope to escape with RLE. Further, the level of forward scatter associated with IOLs is not trivial – it is similar to that of a mild cataract. The effect has been reported by different groups who looked at various IOLs and at different follow-up times (3)(4)(5)(6); in all cases, post-RLE eyes had OSI values in excess of 1.0 – so patients who start with an OSI above 1.0 will again have an OSI above 1.0 after the RLE procedure. Results from our own studies and from the investigations of others (7)(8) have indicated that OSI can be as high as 2.3 in post-RLE eyes (Table 2, a, b).
My second concern with RLE is that current IOLs do not restore accommodation or effectively treat presbyopia. When considering vision across distance, intermediate and near, the only systems that work are micro-monovision or multifocal IOLs. And although multifocal IOLs offer the best outcome, they come with a key disadvantage: photic phenomena. And the problem is bigger than most people realize.
Photic phenomena are among the commonest reasons for patient dissatisfaction with IOLs (9)(10)(11), but this fact is sometimes obscured by the very low self-reported incidence of dysphotopsia (0.2–1.5 percent). When you proactively ask patients about dysphotopsia symptoms, you find that the real incidence is between 20–77 percent. In other words, about half of IOL recipients have some photic phenomena (12)(13)(14)(15)(16)(17). This frequency of visual disturbance is even supported by statements on multifocal IOL package inserts, with glare and halo incidence alone reported to be about 20 percent (18)(19).
Collectively, the weight of evidence suggests that RLE fails to improve symptoms of DLS. So why are we recommending a procedure that has little benefit? I think the actual situation is worse still: RLE may actively increase risks for patients.
Increasing risks
We should remember that IOL implantation is not risk-free. Retinal detachment (RD) may be a particular concern. In the general population – those who have not received ocular surgery – the RD risk is very low (0.0061–0.0179 percent per year). For those who have undergone phacoemulsification the risk rises, reaching 3.6 percent over a follow-up period of four months to two years. Even more tellingly, data from over 200,000 patient records have indicated that operated eyes have a five-fold higher risk of RD following surgery compared with non-operated eyes, and this risk remains elevated for 10 years following surgery (20). And younger, more myopic patients – that is, the ones who are most likely to elect for RLE procedures – actually have a 25-fold higher risk of RD than the standard cataract patient (21). Moreover, because they are younger patients, this risk is elevated for a much longer proportion of their lifetime than an older patient.
We also need to consider IOL decentration – which can occur in around 25 percent of all cataract patients – and dislocation. The frequency of dislocation increases over time: at 10 years there is a one percent risk of IOL dislocation requiring surgery, a 0.7 percent risk of pronounced pseudophakodonesis and a 1.4 percent risk of moderate pseudophakodonesis (22). Concerningly, the frequency of IOL dislocations seems to be increasing (23): in a retrospective cohort study of 140 eyes, the cumulative risk of late dislocation was found to be significantly higher (p<0.001) in patients who were operated on between 2002 and 2012 compared with patients who had IOLs implanted between 1992 and 2001. We must conclude that some aspect of more recent IOL procedures increases the subsequent dislocation risk; we don’t know the cause, but we should be aware of the effect – and advise our patients accordingly.
Optical quality
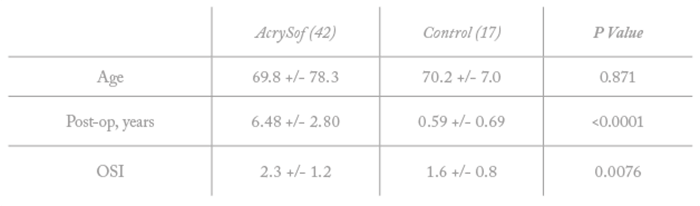
Finally, we should remember that the optical quality of an implanted IOL is not constant, but degrades after implantation. Acrylic IOLs (such as AcrySof, which has over 100 million implantations worldwide) are known to develop significant glistenings (microvacuoles) and whitenings (sub-surface nanoglistenings) over time (24)(25). At three years, around 90 percent of patients will have glistenings on their implanted IOL, with moderate to severe grade glistenings occurring in over 60 percent of patients (26)(27)(28)(29)(30)(31). One study has suggested that glistening-induced light scattering can continue to increase in AcrySof lenses for 15 years post-operatively (32). One study has even shown that five years after AcrySof implantation, 43 percent of patients reported difficulties with night driving and modified their driving habits accordingly (33). Our own research has indicated that AcrySof-implanted subjects are more likely to have self-reported road traffic accidents at five years, and worse visual acuity, than patients implanted with Tecnis IOLs (Table 3). What’s more, evidence suggests that removing the AcrySof lens ameliorates the increased risk of RD, disability glare and IOL dislocation; our data from five patients has shown that visual acuity is improved when IOLs with severe glistening and whitening are exchanged for clear IOLs (24). Similarly, explantation of multifocal acrylic IOLs with glistenings in the optic, and replacement with monofocal IOLs, resolved symptoms and improved visual acuity by up to 4 lines (36).
Conclusions
My strong feeling is that it is time to rethink the RLE procedure. I recognize that I may be ‘swimming against the tide’ – but I am not swimming alone. The problems with RLE have started to become apparent to those who think about these matters. For example, this very issue was raised last year by a colleague in Mexico who frequently participates in clinical trials involving innovative lenses, and therefore sees results that may not be well-publicized. It is interesting that Alcon has very recently introduced a glistening-free lens; perhaps this could be read as an acknowledgement of the problems associated with the current generation of IOLs.
In summary, my basic premise is that RLE is not as safe or effective as we believe, and we need to collectively sit back, look at all the data and think again about how it is used. I am not against IOL procedures altogether – but I certainly try to dissuade young patients with clear lenses from electing for RLE. I show them all the data and tell them about the potential problems, and try to persuade them to try contact lenses or even corneal surgery instead. My experience has been that most patients, when presented with the data, decide against the RLE procedure – and I think that’s wise.
References
- S Schallhorn et al., “Refractive lens exchange in younger and older presbyopes: comparison of complication rates, 3 months clinical and patient-reported outcomes”, J Cataract Refract Surg 43, 737-747 (2017). PMID: 28894356 W Bethke. “Does your patient have a dysfunctional lens?” Available at: http://bit.ly/DysLens. Accessed September 7, 2018. H Lee et al., “Double-pass system assessing the optical quality of pseudophakic eyes”, Optom Vis Sci, 91, 437-43 (2014). PMID: 24492759. A Castillo-Gomez et al., “Evaluation of image quality after implantation of two diffractive multifocal intraocular lens models”, J Cataract Refract Surg, 35, 1244-50 (2009). PMID: 19545816 H Lee et al., “Evaluation of optical quality parameters and ocular aberrations in multifocal intraocular lens implanted eyes”, Yonsei Med J, 55, 1413-20 (2014). PMID: 25048505. MA Nanavaty et al., “Influence of different acrylic intraocular lens materials on optical quality of vision in pseudophakic eyes”, J Cataract Refract Surg, 37, 1230-8 (2011). PMID: 21601419. GH Beiko et al., “A comparison of mesopic visual acuity and objective visual quality following cataract surgery with hydrophobic acrylic intraocular lenses”, Clin Ophthalmol, 11, 641-646 (2017). PMID: 28435215. S Beheregaray et al., “Influence on visual function of forward light scattering associated with subsurface nanoglistenings in intraocular lenses”, J Cataract Refract Surg, 40, 1147-54 (2014). PMID: 24874769. MA Woodward et al., “Dissatisfaction after multifocal intraocular lens implantation”, J Cataract Refract Surg, 35, 992–997 (2009). PMID: 19465282. NE de Vries et al., “Dissatisfaction after implantation of multifocal intraocular lenses”, J Cataract Refract Surg, 37, 859–865 (2011). PMID: 21397457. NE de Vries and RM Nuijts, “Multifocal intraocular lenses in cataract surgery: Literature review of benefits and side effects”, J Cataract Refract Surg 39, 268–278 (2013). PMID: 23332253. T Aslam et al., “Long-term prevalence of pseudophakic photic phenomena”, Am J Ophthalmol 143, 522-24 (2007). PMID: 17317404. P Bournas et al., “Dysphotopsia after cataract surgery: comparison of four different intraocular lenses”, Ophthalmologica 221, 378-83 (2007). PMID: 17947823. J Davison. “Positive and negative dysphotopsia in patients with acrylic intraocular lenses”, J Cat Refract Surg, 26, 1346-55 (2000). PMID: 11020620. W Meacock et al., “The effect of texturing the intraocular lens edge on postoperative glare symptoms: a randomized, prospective, double-masked study”, Arch Ophthal 120, 1294-98 (2002). PMID: 12365907. S Shambhu et al., “The effect of lens design on dysphotopsia in different acrylic IOLs”, Eye, 19, 567-70 (2005). PMID: 15389285. R Tester et al., “Dysphotopsia in phakic and pseudophakic patients: incidence and relation to intraocular lens type”, J Cat Refract Surg, 26, 810-16 (2000). PMID: 10889424 Alcon Laboratories. “AcrySof ReSTOR IQ Multifocal IOL”. Available at: http://bit.ly/AcrysofPI. Accessed September 7, 2018. Updated DFU for the Tecnis multifocal foldable acrylic intraocular lens. Available at: http://bit.ly/TecnisDFU. Accessed September 7, 2018. M Dela Cour, presented at German Ophthal Soc Meeting, 2016. V Daien et al., “Incidence, risk factors, and impact of age on retinal detachment after cataract surgery in France2, Ophthalmology, 122, 2179-85 (2015). PMID: 26278859 EI Monostam. “Incidence of dislocation of intraocular lenses and pseudophakodonesis 10 years after cataract surgery”, Ophthalmology, 116, 2315-20, (2009). PMID: 19815277. K Dabrowska-Kloda et al., “Incidence and risk factors of late in-the-bag intraocular lens dislocation: Evaluation of 140 eyes between 1992 and 2012”, J Cataract Refract Surg, 41, 1376-82 (2015). PMID: 26187678. H Matsushima et al., “Decreased visual acuity resulting from glistening and sub-surface nano-glistening formation in intra-ocular lenses: A retrospective analysis of 5 cases”, Saudi J Ophthalmol 29, 259-63 (2015). PMID: 26586975. A Behndig and E Monestam, “Quantification of glistening in intraocular lenses using Scheimpflug photography”, J Cat Refract Surg, 35, 14-7, (2009). PMID: 9101419. H Minami et al., “Glistening of Acrylic Intraocular Lenses”, Rinsho Ganka (Jpn J Clin Ophthalmol), 53, 991-994 (1999). J Colin and I Orignac, “Glistenings on intraocular lenses in healthy eyes: effects and associations”, J Refract Surg, 27, 869-75 (2011). PMID: 21800784 J Colin et al., “Glistenings in a large series of hydrophobic acrylic intraocular lenses”, J Cataract Refract Surg, 35, 2121-6 (2009). PMID: 19969218. E Mönestam and A Behndig, “Impact on visual function from light scattering and glistenings in intraocular lenses, a long-term study”, Acta Ophthalmol, 89, 724-8 (2011). PMID: 20064111. E Peetermans and R Hennekes, “Long-Term Results of Wagon Wheel Packed Acrylic Intraocular lenses (AcrySof)”, Bull Soc. Belge Ophtalmol, 271, 45-48 (1999). PMID: 10355159. C Leydolt et al., “Posterior Capsule Opacification with the iMics1 NY-60 and AcrySof SN60WF 1-Piece Hydrophobic Acrylic Intraocular Lenses: 3-Year Results of a Randomized Trial”, Am J Ophthalmol, pii: S0002-9394(13)00251-1. doi: 10.1016/j.ajo.2013.04.007 (2013). PMID: 23677137. K Miyata et al., “Effect of visual acuity of increased surface light scattering in intraocular lenses”, J Cat Refract Surg, 38, 221-6 (2012). PMID: 22322162. E Monestam and B Lundqvist, “Long-time results and associations between subjective visual difficulties with car driving and objective visual function 5 years after cataract surgery”, J Cataract Refract Surg 32, 50-55 (2006). PMID: 16516778. GH Beiko, “A pilot study to determine if intraocular lens choice at the time of cataract surgery has an impact on patient-reported driving habits”, Clin Ophthalmol, 9, 1573-79 (2015). PMID: 26357458. GH Beiko et al., “A comparison of mesopic visual acuity and objective visual quality following cataract surgery with hydrophobic acrylic intraocular lenses”, Clin Ophthalmol, 11, 641-646 (2017). PMID: 28435215. M van der Mooren et al., “Explanted multifocal intraocular lenses”, J Cataract Refract Surg, 41, 873-877 (2015). PMID: 25840309.
