Peer-Reviewed Study Shows Optometrists and Ophthalmologists Frequently Miss Macular Degeneration
By Jeffry Gerson, OD, and Mark F. Pyfer, MD
A recent study published in JAMA Ophthalmology revealed how frequently optometrists and ophthalmologists fail to diagnose age-related macular degeneration (AMD) (1). The cross-sectional study, which included 1288 eyes (644 adults) from patients enrolled in the Alabama Study on Early Age-Related Macular Degeneration (ALSTAR) (2)(3), revealed that doctors are missing AMD about 25 percent of the time. Also quite concerning is that 30 percent of the undiagnosed eyes in the study had large drusen, a known risk factor for wet AMD (1).
Understanding The Study
The authors set out to determine to what extent AMD is under-diagnosed by primary eye care physicians when the disease is actually present. In the study, they reviewed the medical records of 644 adults 60 years or older who were enrolled in ALSTAR. To be eligible, the person’s medical record from the most recent comprehensive dilated examination did not indicate a diagnosis of AMD in either eye, and the medical record notes did not contain terms that signified the signs of AMD. Each patient in the ALSTAR study had digital color fundus photos taken, which were reviewed by masked, trained graders who determined the presence or absence of AMD findings according to the Clinical Age-Related Maculopathy Staging (CARMS) system (4). The types of AMD-associated lesions also were noted.
The results revealed that one of four eyes studied was not diagnosed with AMD during the dilated fundus examination, despite these eyes having macular characteristics indicative of AMD in the fundus photos. Approximately three-fourths of the 320 undiagnosed eyes had 10 or more small drusen (249 [77.8 percent]) and/or intermediate drusen (250 [78.1 percent]), with 96 (30.0 percent) of undiagnosed eyes having large drusen.
Who Overlooks AMD?
“As this study reveals, even the most experienced and well-trained primary eye care doctors can miss AMD, which may result in severe vision loss,” says Jeffry Gerson, OD. “In fact, the prevalence of undiagnosed AMD in the study was not different for ophthalmologists versus optometrists.”
Although the study authors say reasons for the missed diagnoses remain unclear, they point out that improved AMD detection strategies may be needed in primary eye care since many of these patients would have been candidates for therapeutic intervention with nutritional supplements.
“Current technology may lead to a sense of complacency, and does not always enable us to detect AMD early enough. This is easily overcome when dark adaptation testing is available,” says Dr. Gerson.
The authors also call attention to potential treatments for earlier stages of dry AMD that will likely be developed in the coming years.
“While there is no cure for early AMD, it is important to diagnose the disease as early as possible to increase monitoring, educate patients and start measures that may slow progression. We can recommend lifestyle changes, such as smoking cessation, exercise and a healthy diet including antioxidant vitamins, and UV light protection with sunglasses as a start,” says Mark F. Pyfer, MD. “Doctors who have the tools needed for earlier detection have a tremendous opportunity to help their patients, and advance their practices.”
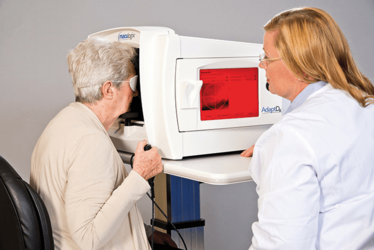
Testing dark adaptation function with the AdaptDx® can help diagnose AMD at least three years earlier than drusen are visible.
The Road To Improved Outcomes
The challenge is that many cases of AMD are overlooked based on the absence of structural findings using some of the most advanced technology. For example, Ocular Coherence Tomography (OCT) is essential for detecting and managing many retinal diseases, but it only looks at structure. “Depending on interpretation, the OCT scan of a patient with a few small drusen is often normal and potentially underestimates the extent of disease,” says Dr. Pyfer. “By the time photoreceptor ellipsoid layer thinning is visible on OCT, macular function may be significantly impaired.” He adds: “Dark adaptation testing with the AdaptDx is a straightforward adjunct to OCT, fundus photography and standard clinical examination. This functional test allows you to detect AMD at least three years before it becomes clinically evident” (5). Several peer-reviewed studies have shown that dark adaptation function is dramatically impaired from the earliest stages of AMD, with increasing impairment as the disease progresses (6)(7).
Did You Know?
- Up to 78 percent of AMD patients have substantial, irreversible vision loss at first treatment, including 37 percent who are legally blind in at least one eye (10)(11)
- Unlike macular pigment optical density (MPOD) testing or genetic tests, the AdaptDx does not measure AMD risk. This easy-to-perform test is diagnostic of AMD, indicating that disease is already present
In a recently published study, subjects with impaired dark adaptation were twice as likely to develop clinically evident AMD and eight times as likely to advance beyond the earliest stage of AMD (8). The only commercially available automated dark adaptometer, called the AdaptDx, measures a patient’s Rod Intercept (RI) time. RI is the number of minutes it takes for the eye to adapt from bright light to darkness at a standard threshold stimulus level. The AdaptDx test provides a clear and objective measurement of retinal function with 90 percent sensitivity and specificity (9). An RI of less than 6.5 minutes indicates normal dark adaptation consistent with healthy photoreceptor function. An RI greater than 6.5 minutes indicates impaired dark adaptation, most often due to AMD in patients over age 50, unless there is a pre-existing hereditary retinal degeneration or significant vitamin A deficiency, which is rare in the United States.
“This study is a real eye-opener that clearly shows that, without the necessary technology, ODs and MDs are not always able to deliver the level of care that we would want for ourselves, our families and, of course, our patients,” says Dr. Gerson. “The good news is that new technology can make it easier for us to walk out of the exam room with greater confidence in our diagnosis and our patient’s prognosis.”
Jeffry Gerson, OD, FAAO, practices at Grin Eye Care in Olathe, KS. He is a fellow of both the Academy of Optometry and Optometric Retina Society. Mark F. Pyfer, MD, FACS, is a cataract and refractive surgeon at Northern Ophthalmic Associates in Jenkintown, PA. He serves on the teaching faculty at Wills Eye Hospital in Philadelphia.
- DC Neely et al. “Prevalence of Undiagnosed Age-Related Macular Degeneration in Primary Eye Care”, JAMA Ophthalmol. 135, 570-575 (2017). PMID: 28448669.
- C Owsley et al., “Associations between abnormal rod-mediated dark adaptation and health and functioning in older adults with normal macular health”, Invest Ophthalmol Vis Sci, 55, 4776-4789 (2017). PMID: 24854857.
- C Owsley et al., “Comparison of visual function in older eyes in the earliest stages of age-related macular degeneration to those in normal macular health”, Curr Eye Res, 41, 266–272 (2016). PMID: 25802989.
- JM Seddon, S Sharma, RA Adelman, “Evaluation of the clinical age-related maculopathy staging system”, Ophthalmology, 113, 260–266 (2006). PMID: 16458093.
- C Owsley et al., “Delayed Rod-Mediated Dark Adaptation Is a Functional Biomarker for Incident Early Age-Related Macular Degeneration”, Ophthalmology, 123, 344–351 (2015). PMID: 26522707.
- C Owsley et al., “Delays in rod-mediated dark adaptation in early age-related maculopathy” Ophthalmology, 108, 1196–1202 (2001). PMID: 11425675.
- CA Curcio, M Johnson, “Structure, function, and pathology of Bruch’s membrane”. In: Ryan SJ, et al, eds. Retina, Vol 1, Part 2: Basic Science and Translation to Therapy. 5th ed. London: Elsevier; 466–481 (2013).
- C Owsley et al., “Delayed Rod-Mediated Dark Adaptation is a Functional Biomarker for Incident Early Age-Related Macular Degeneration”, Ophthalmology, 123, 344–351 (2016). PMID: 26522707.
- GR Jackson et al., “Diagnostic Sensitivity and Specificity of Dark Adaptometry for Detection of Age-Related Macular Degeneration”, Invest Ophthalmol Vis Sci, 55, 1427–1431 (2014). PMID: 24550363.
- RA Cervantes-Castañeda et al. “Lack of benefit of early awareness to age-related macular degeneration”, Eye, 22, 777–781 (2008). PMID: 17220824.
- TW Olsen et al., “Fluorescein angiographic lesion type frequency in neovascular age-related macular degeneration”, Ophthalmology. 111, 250–255 (2004). PMID: 15019371.













