
TrabEx Pro: The Next Level in MIGS
A longtime Trabectome user outlines the advantages of the new TrabEx Pro

contributed by MST |
MST’s Trabectome - invented by the late Dr. George Baerveldt - was the first MIGS device approved by the FDA in 2004. UC Irvine’s Dr. Sameh Mosaed performed the very first case in the US; in 2015, Dr. Mosaed wrote a 10-year review of the global Trabectome experience. Now, nearly 20 years on from Trabectome’s introduction, ophthalmologists “have had ample clinical experience with the device,” says Ken Lin, Associate Clinical Professor and Director of Medical Education at UC Irvine’s Ophthalmology School of Medicine. And, he explains, “few other MIGS can rival Trabectome in the quantity and quality of clinical studies.”
Lin has a busy glaucoma practice at UCI; his research focuses on using deep learning and artificial intelligence to enhance various surgical and clinical aspects of glaucoma. His lab has developed a deep learning system that accurately identifies the trabecular meshwork in real-time under gonioscopic view; it also develops prototypes for microsurgical devices for glaucoma.
As a Trabectome user for more than ten years, Lin believes the most notable MIGS development of the last decade is the extensive array of options to bypass or ablate the trabecular meshwork. For three subtypes of open angle glaucoma - steroid-induced, pigmentary, and pseudoexfoliative glaucoma - the trabecular meshwork is the primary site of resistance and as such, removing it cleanly with a device such as the Trabectome can effectively lower the IOP, he explains. Lin has also tried to “maximize the treatment area with Trabectome, as the pressure reduction is directly correlated to the treatment area.”
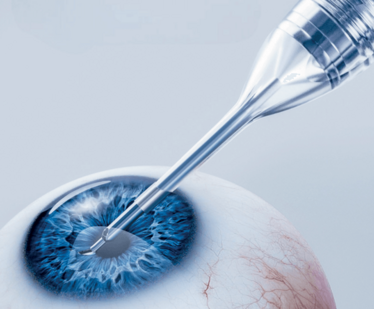
MST recently extended its line of goniotomy devices with TrabEx Pro, which includes innovative features that facilitate a more complete excision of diseased trabecular meshwork. The device features a trapezoidal blade head with laser-honed serrated blades, allowing for a custom cut for each individual patient and each section of tissue.
Significantly, TrabEx Pro is compatible with all phacoemulsification platforms. One of Lin’s concerns about Trabectome, for example, has been the cost. “The console does require a significant capital equipment purchase,” he explains. However, “as a single-use device that easily attaches to all phaco platforms, TrabEx Pro retains most of Trabectome’s features and strengths without the significant financial investment upfront.”


Lin started using TrabEx Pro in February 2023, and was “very impressed with its ease of use.” In the past, he typically utilizes Trabectome after the intraocular lens is placed into the capsular bag and uses a large 2.7mm incision for phacoemulsification. As such, he needs to place a temporary 10-0 vicryl suture to make his main incision small enough to insert the Trabectome handpiece; otherwise, the irrigation will reflux out of the main incision site. However, with TrabEx Pro, “the silicone sleeve snugly seals the main wound without impeding on the handpiece’s maneuverability,” he explains. “This saves me from having to place a suture. In addition, the design of the blade tip is such that it glides against the back-wall of Schlemm’s canal very smoothly.”

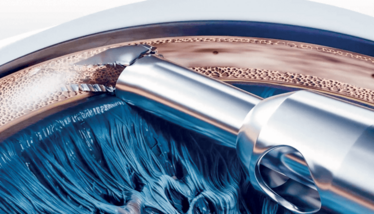
“TrabEx Pro is the only device on the market - other than Trabectome - that provides irrigation and aspiration,” he observes. “This is very important as blood reflux often makes angle procedure difficult to perform precisely; commonly, only a small area is treated due to poor view.” Furthermore, Lin finds TrabEx Pro’s high vacuum visco setting “very effective” in removing the trabecular strands that sometimes stay adherent to the angle, which if left in the eye, may promote synechiae to form across the trabecular cleft.
Lin says that his operating room staff “all raved about how easy it is to set up TrabEx Pro and how responsive the MST team has been.” In his early experience with TrabEx Pro, he can confirm that he is seeing an average IOP reduction of 30% - with many patients becoming drop-free after the procedure. “Of the small sample of patients so far,” he concludes, “I can see that their results are comparable with those of Trabectome patients.”
Log in or register to gain full unlimited access to all content on the The Ophthalmologist site. It’s FREE!













