Shifting to a Systemic Approach
What does the future hold for the management – and treatment – of diabetic eye disease?

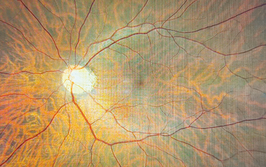
The prevalence of diabetic eye diseases is increasing worldwide. Given that diabetic macular edema (DME) is a major cause of vision loss in diabetes patients, screening is more important than ever. Thankfully, a number of artificial intelligence systems have been developed in recent years for autonomous detection of diabetic retinopathy (DR) and DME, including the IDx system, which can be used to detect DR with a sensitivity of 87.2 percent and a specificity of 90.7 percent.
The test only takes a few minutes and can be done in the primary care physician’s office, increasing our ability to detect disease early – and it provides diagnostic interpretation and care instructions aligned with American Academy of Ophthalmology guidelines for DR. In April 2018, IDx-DR was approved by the FDA for the detection of greater than mild level of DR in adults who have diabetes and can now be found in endocrinology clinics, internal medicine clinics, diabetes education centers, diagnostic labs, community health clinics and diabetes research groups (1).
Another important topic is the role of OCTA. We know that OCT allows us to detect the most minuscule changes in retinal thickness and hydration. It serves as the most important tool in the monitoring of patients treated for DME, and provides the data we need to make treatment and retreatment decisions. OCTA, while providing data on macular perfusion and blood flow, has not yet been shown to be crucial for the management of the disease and is, at this time, still optional (2).
Home monitoring devices, such as home OCT, have the potential to improve patient management, and appear to provide excellent images when self-operated by elderly patients. In combination with automated analysis of hydration and fluid, such devices could improve patient care while reducing the burden of visits on the physician and the patient (3).
Considering pharmacotherapy, the anti-vascular endothelial growth factor (VEGF) substances available on the market have shown consistently good efficacy and safety, and have thus become the standard of care. But as always, even the most advanced treatment has its limits, and results for anti-VEGF do vary according to baseline visual acuity, subretinal fluid (SRF) and intraretinal cystoid fluid (IRC), amongst other factors (4). Moreover, anti-VEGF entails high costs, and frequent visits to the clinic. Steroids are also widely-used for DME, most typically as a second-line treatment. But, as dexamethasone implants allow fewer visits to the clinic, they may also be used as a first-line treatment among patients who are unwilling or unable to visit the clinic as often as needed for anti-VEGF treatment (5).
But steroids and anti-VEGF are not the only avenues being explored. Faricimab, a bispecific monoclonal antibody, has already been shown as a therapy with potential for a longer duration of effect in DME (6). Other drugs, such as abicipar and brolucizumab, have also been shown to assist in the treatment of AMD, are now being investigated for DME (7, 8). Slow release devices, such as the PDS, have been found effective in cases of AMD, and certainly have the potential to solve the burden and frequent injections issue associated with DME (9).
Despite welcome progress in treatment and technology, issues remain. In my view, systemic diseases, such as diabetes, are crying out for systemic approaches – including coordination with the patient’s medical team. Shifting in this direction may prove challenging but, if we want to deliver the highest quality care, shift we must.
The author discloses that she is a consultant to Allergan, Bayer Healthcare, Beyeonics, Forsightlabs, Notal Vision, Novartis and Roche.
- M Abràmoff et al., “Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices”, NpJ Digital Medicine, 1, 39 (2018). PMID: 31304320.
- D Gildea, “The diagnostic value of optical coherence tomography angiography in diabetic retinopathy: a systematic review”, Int Ophthalmol (2018). PMID: 30382465.
- K Miller et al., “Home monitoring for age-related macular degeneration”, Curr Ophthalmol Rep, 6, 53 (2018).
- S Bressler et al., “Factors associated with visual acuity and central subfield thickness changes when treating diabetic macular edema with anti-vascular endothelial growth factor therapy: an exploratory analysis of the protocol T randomized clinical trial”, JAMA Ophthalmol 137, 382 (2019). PMID: 30676635.
- D Zur et al., “The role of steroids in the management of diabetic macular edema”, Ophthalmic Res (2019). PMID: 31048580.
- J Sahni et al., “Simultaneous inhibition of Angiopoietin-2 and vascular endothelial growth factor-A with Faricimab in diabetic macular edema: BOULERVARD phase 2 randomized trial”, Ophthalmology, 126, 1155 (2019). PMID: 30905643.
- D Callanan et al., “Double-masked, randomized, phase 2 evaluation of abicipar pegol (an anti-VEGF DARPin therapeutic) in neovascular age-related macular degeneration”, J Ocul Pharmacol Ther, 34, 700 (2018). PMID: 30412448.
- P Dugel et al., “HAWK and HARRIER: phase 3, multicenter, randomized, double-masked trials of brolucizumab for neovascualr age-related macular degeneration”, Ophthalmology (2019). PMID: 30986442.
- P Campochiaro et al., “The port delivery system with ranibizumab for neovascular age-related macular degeneration: results from the randomized phase 2 Ladder clinical trial”, Ophthalmology, 126, 1141 (2019). PMID: 30946888.
Anat Loewenstein, MD, MHA, is a professor and director of the Department of Ophthalmology, Vice Dean of the Faculty of Medicine, and Sidney Fox Chair of Ophthalmology at Tel Aviv University. She is also Chairman of Ophthalmology at Sourasky Medical Center in Tel Aviv and President of the Israeli Ophthalmological Society.
Disclosures: Anat Loewenstein is a consultant to to Allergan, Bayer Healthcare, Beyeonics, Forsightlabs, NotalVision,Novartis, Roche, Syneos, Xbrane, Nanoretina, Ocuterra, Ripple Therapeutics, Annexon, MJHEvents, Iveric Bio, Biogen, Johnson & Johnson, Ocuphire Pharma, and Iqvia.