
Robot Dreams
The UK’s NIHR recently awarded £1,000,000 to a project led by Research Scientist, Christos Bergeles, and Consultant Ophthalmic Surgeon, Lyndon da Cruz
At a Glance
- The challenge for retinal cell therapy is positioning the therapeutic cells very precisely into the correct retinal layers
- A collaborative project team is working on developing a device that provides the surgeon with delivery tubes capable of multiple orientations and flexibility of operation
- The human factor is important to the researchers, who have been involving patients, and the broader public, in discussions about medical robotics
- Patient representative, Douglas Tredget, shares his experience of being part of the robotics project.
At King’s and MEH, part of our remit is to develop clinically-relevant technology that will enhance the National Health Service’s capabilities. Developing a novel robotics system to enable very precise retinal manipulations is a great example. The idea is to improve operating room technology and – in particular – bring it up to speed with cell therapy, so that regenerative medicine for the retina can achieve its full potential.
Regenerate the degenerating
What made us commit to the project? In brief, an opportunity and a challenge. The opportunity is to help cure diseases that cause blindness. Today, gene and stem cell therapies have the potential not just to delay but also to reverse degenerative eye diseases – this is borne out by recent work on gene therapy for choroideremia and cell therapy for age-related macular degeneration (1). However, for retinal cell therapy to reach its full potential, therapeutic cells must be able to be positioned very precisely into the correct retinal layer – and this is the challenge we take on.
Current systems for delivering cells to the retina simply have not caught up with the advances – and requirements – of cell therapy. In fact, delivery systems such as manually-operated needles remain somewhat crude and limited by the physical capabilities of humans in terms of precision and tremor. This in turn limits the development of cell therapies. It is frustrating that the therapeutic cells exist but cannot be delivered to the 10-micron zone in the retina where they are needed. The technology to enable such precision does not currently exist. We realize that we are at the limits of what the human hand can achieve, and this is impeding the translation of cell and molecular therapies into the clinic.
Beyond dexterity
The realization that the human hand may hold back advances in cell therapy led the two of us, Lyndon and Christos, to initiate this collaborative project. The combination makes an ideal team, one of us leading the engineering component, while the other leads the clinical surgical translation aspect. Our fundamental aim is to enable precise and reliable micro-scale retinal surgery for cell therapy.
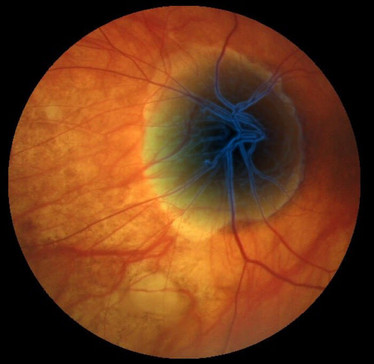
In more detail, the problem we face is not just one of scale, but of relative scale. Consider: the status quo of retinal surgery involves a linear instrument that enters the eye through the sclera, the white of the eye; thereafter, any surgical manipulations require the instrument to pivot around that entry point. Assume, for the sake of argument, that the depth of the eye – from scleral entry point to retina – is 1 cm, and the target zone is 10 microns (0.01 mm). And that equates to a thousand-fold difference in size between the instrument length and the target zone. In other words, the surgeon is attempting the equivalent of hitting a one-meter target with a one-kilometer pole! The disparity between distance and required precision was a key problem for us to overcome.
Our solution? In effect, to move the pivot point closer to the target – essentially, to provide the linear instrument with a flexible tip. Briefly, our device comprises a linear outer tube containing smaller, deformable inner tubes (Figure 1), fabricated from a memory material (NiTi CC). The inner tubes can be pushed out of the end of the device; once outside, their tips take on the shape in which they were fabricated. Similarly, upon retraction they deform so as to fit into the outer tube. The tips are designed to facilitate micro-incisions and delivery of viable cells. In addition, the tips can be rotated as required to assist with precise cutting and targeted implantation. The device therefore provides the surgeon with delivery tubes capable of multiple orientations and unparalleled flexibility of operation.

Figure 1. Main components and architecture of the robotic system. An actuation system transmits motion to the flexible tip through an array of concentric cylinders (like pistons). This way, the actuation system is decoupled from the tip, and enables changing the tip during surgery.
Helping hands
Our project has involved several individuals focusing on different elements of the technology. Initial tasks included development of custom software to achieve the required device tip flexibility, and development of novel actuation components and stabilisation constraints. Ongoing work includes perfection of image processing systems to better guide the surgeon , and construction of advanced electromechanical control and feedback systems. And before all of this innovation, we had to cover a lot of background work; for example, to ensure that we were completely familiar with anatomical landmarks of the eye and how they can guide surgery.
As with any translational project, problems arose as development proceeded. Throughout, we have had to consider many aspects: the sterility of the device; how to drape the instrument; components that should be single use; and the cost implications of all the above. Safety is key, of course – we must allow for the unexpected, and ensure that if there is any kind of intra-operative failure, the device can be fully controlled and carefully retracted at all times. Nobody wants to see a medical robot run amok! All these aspects must be managed, and they add to the project timelines. Fortunately, we’ve had no major problems, and the funders remain happy with our progress.
That said, with robotic systems you can theorise as much as you like, but you won’t know if they work until you build them. We are now making prototypes for evaluation in model systems, such as plastic eyes. The resulting data will allow us to improve the device and bring it closer to clinical application. And as we expect this surgery to be performed under local anesthesia, we are also going to develop image stabilisation algorithms to cancel out patient movements – not just breathing, but also head movements. Vitreoretinal surgery is currently, normally, done under local anesthesia, and we want to stick as closely as possible to existing practices!
Real-world impact
The increased precision permitted by our system will assist conventional retinal surgery to some extent – for example, it will make retinal membrane peeling or vessel cannulation a little faster and safer. However, conventional surgery is already highly reliable, so the improvement afforded by our system would only be incremental – say, a move from 90 to 95 percent efficacy. The real importance of our system will be in enabling forms of surgery that are at present impossible – namely, the precise localised delivery of gene or cell therapies to any individual retinal layer.
As well as optimizing the engineering and surgical effect, we are trying to maximise our real-world impact by involving patients, and the broader public, in discussions about medical robotics. It is important for researchers – and clinicians – to be aware of the human factor, no matter how exciting the technology. Understanding people’s hopes and fears and incorporating these into research is why patients like Douglas Tredget (see interview below) are so valuable. Not only do they offer tremendously helpful insights through lived experience, but they can quickly raise issues that could otherwise take us years to recognise.
We are very happy with the progress we have made – the project has been running for about one year now, and has attracted financial support over and above the original National Institute for Health Research (NIHR) grant. It has just grown and grown, which makes everybody happy, including the original funders. Above all, we look forward to making a real difference to patients with degenerative disorders of the eye. The days of therapeutic delivery by handheld needle are numbered!
Augmented reality for effective image-guided ophthalmic surgery
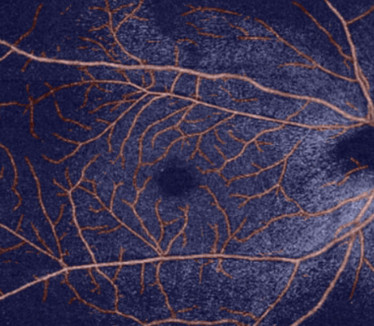
Claudio Ravasio, a PhD student, is developing systems to enhance the surgeon’s intra-operative view of the retina. Theodoros Pissas, a PhD student, identifies critical landmarks on optical coherence tomography angiography images.
- Integration of images of different retinal layers will assist intra-operative manipulations
- Based on near-real time, ‘inverse realism’ computer-generated images, the system will combine optical microscopy and pre-operative optical coherence tomography (OCT) images
- Surgeons will access augmented images via 3D screen or head-mounted display
- Integration with robotic operating system will enable surgeons to position device tip very accurately
- It will reduce training time, increase safety, simplify navigation, increase precision.
Hardware integration and telemanipulation
John O’Neil, alumnus post-doctoral researcher, developed electromechanical control and feedback systems
- Desk model prototype: electric motors advance and retract internal tubes within delivery device
- Surgeon controls tube movements via a joystick system
- Forthcoming: control system that gives surgeon physical feedback through hand-held joysticks

Figure 2. Christos Bergeles, Douglas Tredget and Lyndon da Cruz.
How the patient sees it
Douglas Tredget is the Macular Society patient representative on the King’s/UCL/Moorfields Eye Hospital robotics project.
What is your experience of AMD?
I was diagnosed with AMD in 1998. After noticing a blurred spot in the vision of one eye, I contacted my local ophthalmologist, who sent me to the West Kent Eye Hospital. Subsequently, I was referred to Professor Bird and Dr Tufail at Moorfields Eye Hospital, London. Currently I am being treated by Tim Jackson at King’s College Hospital, London.
In the last five years, I have joined the Kent Association for the Blind (KAB); I do voluntary work for them and have befriended a gentleman with AMD at a more advanced stage than mine. I also participate in bridge games for partially sighted people, again at KAB, and I know a number of other AMD patients via my local Macular Society.
Why did you get involved with the Macular Society and this robotics project?
I joined the Macular Society to keep abreast of research and to participate in clinical studies. For example, I have been involved with investigations into the effects of diet, aspects of facial recognition, and methods of vision assessment. Recently, the Society asked me if I would be interested in this robotics project. I agreed, and the project leaders – Christos Bergeles and Lyndon da Cruz – got in touch with me and explained the project aims and timelines. They also introduced me to the other members of the team.
Since then, I’ve been sitting in on the robotics project quarterly progress meetings, where different members of the team present their work and new research results. Sometimes the researchers demonstrate the robot prototypes they are working on. Following these meetings, I write summary articles for Sideview (the magazine of the Macular Society) about different aspects of the research.
What do you think about the technology and its potential impact on patients’ lives?
There are many AMD research projects, but to me this one seems the most likely to succeed. In the first trial of stem cell therapy for AMD (1), about three years ago, Lyndon da Cruz and Pete Coffey (UCL) showed that stem cell implantation into the macular resulted in quantifiable improvement of symptoms. As Lyndon explained at the first project meeting, the biological aspect of this therapeutic approach was sound, but the surgical aspect – the actual delivery of the stem cells – was impeded by human limitations. It was just too difficult for routine application. As Lyndon put it, the macular has many fine layers, a bit like an onion – and we need to deliver the stem cells between these layers, without causing too much damage in the process. It is hoped that robotic systems will be able to carry out this delicate procedure more safely and reliably than manual approaches.
What aspects of the technology most interest you?
The power of computing to bring accuracy and standardization to complex operations! In my own profession, I have had first-hand experience of the ability of computers to increase speed and reliability, and I am excited and encouraged by their application to retinal surgery.
Disclaimer
The research was funded by the NIHR Invention for Innovation Programme. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.

- 1. L da Cruz et al., "Phase 1 clinical study of an embryonic stem cell-derived retinal pigment epithelium patch in age-related macular degeneration", Nat Biotechnol, 36, 328-337 (2018). PMID: 29553577.
- 2. Lin, Fang-Yu, Christos Bergeles, and Guang-Zhong Yang. "Biometry-based concentric tubes robot for vitreoretinal surgery." Engineering in Medicine and Biology Society (EMBC), 2015 37th Annual International Conference of the IEEE. IEEE, 2015.
Christos Bergeles is a Lecturer and Assistant Professor in the Translational Imaging Group in the Centre for Medical Image Computing at University College London’s Department of Medical Physics and Biomedical Engineering.
Lyndon da Cruz works at the NIHR Biomedical Research Centre, Moorfields Eye Hospital and University College London













