FLACS Takes Flak
How does femtosecond laser-assisted cataract surgery really stack up against standard manual procedures?

When FLACS was first adopted in Europe, back in 2006, we had high hopes for this exciting new technology – unfortunately, these hopes have not been met. I say this from the perspective of 15 years’ direct experience of the technique, during which time I have performed hundreds of procedures – including our combined femto and nanosecond laser cataract method, for which we received a video award at the 2015 ASCRS meeting. My opinion therefore has been formed by extensive personal experience of the FLACS method.
One of the first claims made for FLACS was that it mediated a capsulorhexis that was biomechanically superior to that provided by other methods. My view, however, is that the biomechanical rigidity of the FLACS capsulorhexis is not clearly superior to that provided by alternative methods. I make this statement based on outcomes I have seen from both manual capsulorhexis procedures and capsulorhexis procedures using other disposable devices, such as the Zepto. In the light of this evidence, the “biomechanical superiority” claim is difficult to defend.
Similarly, it has been widely suggested that FLACS permits much more precise centration than manual techniques, or even Zepto procedures, thanks to the “made-to-measure” trephination associated with intraoperative, anterior segment OCT technology. We should remember, however, that a FLACS capsulorhexis does not inevitably provide zero decentration: true, positioning often appears perfect in the immediate post-operative period, but capsule fibrosis and phimosis may gradually alter capsulorhexis shape and/or lens position over time. Consequently, the refractive data of these patients need to be evaluated at least a year after the procedure to achieve an accurate picture of the outcome. An additional consideration here is that effective capsulorhexis diameter varies according to capsule elasticity; hence, it is much larger in younger patients, in whom the capsule has more expansion potential. Clearly, this is an important issue: effective anterior capsule overlap is necessary to stabilize the IOL optic and thus avoid movement, decentration, phimosis and reductions in the refractive and astigmatic power of toric IOLs. Indeed, my opinion is that we need more data on this issue, not least to support development of an algorithm to adjust for this effect in younger patients.
Another claimed advantage of FLACS relates to the quality of the corneal incision, which is often said to be dramatically improved by femtosecond laser techniques. This, however, ignores less desirable aspects of laser-mediated corneal incisions. For example, my experience is that FLACS incisions generate a significant number of surprises, depending on their exact location, and that the second small incision tends to “float” (does not reach the corneal surface). Additionally, I have found that FLACS incisions are less watertight than manual incisions, regardless of variations in parameters, such as incision shape. For this reason, in my practice I prefer when applying FLACS to employ a manual blade corneal incision technique following the femto-assisted capsulorhexis and lens fragmentation.
My reservations regarding femtosecond lasers extend to their use in assisted astigmatic keratotomy as an adjunct to cataract surgery. This technique is supported by a significant number of clinicians, especially in the USA, but my impression is that astigmatic keratotomy incisions can be significantly misplaced when mediated by femtosecond laser – they may even approach the visual axis of the patient. Hence, I persist in my belief that astigmatic keratotomy is not the best option for the patient. In fact, I believe it should be the last option; a toric lens should be the first choice, and laser-vision correction with LASIK or PRK the second. A broader point is that astigmatic keratotomies tend to be unstable over the long term; this is probably due to gradual changes in corneal rigidity that alter the effect of previous incisions. This view is supported by my own experience and follow-up of astigmatic keratotomies for over 25 years, and from reports in the peer-reviewed literature.
A particular FLACS-associated problem that frequently arises in our patient population is related to the effect of anesthesia. For the last eight years, we have performed all cataract procedures under a short duration, topical anesthetic. Specifically, we use 10 mL of 1 percent xylocaine, which we make up by a 1:1 BSS dilution of commercially available 2 percent xylocaine. This preparation effectively stops eye movements and sensation for about an hour and offers great comfort for the patient and safety for the procedure. Unfortunately, it makes subsequent use of a femtosecond laser impossible, since the peribulbar anesthetic invariably presents also as conjunctival chemosis, which prevents the patient interface effectively engaging the eye. Thus, FLACS is significantly incompatible with our preferred method of topical anesthesia.
Another issue concerns the amount of energy absorbed by ocular tissues during FLACS and phacoemulsification. Where FLACS is employed, consequences include relatively high levels of iritis and post-operative discomfort, which in turn require additional post-operative treatment – and additional surgeon time. Indeed, the time disadvantage of FLACS is worth emphasizing in itself: in my hands, an IOL implantation requires 10-12 minutes, with a patient turnaround of 10 minutes, whereas a FLACS procedure routinely takes over 30 minutes.
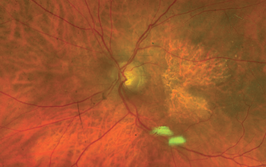
But what about outcomes? After all, these are the most important measures. My own data are clear: visual acuity on day 1 post-surgery is far better with manual than with FLACS techniques, and very similar at one year after surgery. My conclusion is that FLACS has no clinical advantage over manual surgery, at least not in the cases I have treated. In fact, my experience is that FLACS carries risks over and above those of manual techniques, including inadvertent capsular tears; these can cause significant stress and demand additional operating time. It’s true that FLACS and Zepto reduce the chances of getting an “Argentinian flag” sign after scoring the anterior capsule, but this complication is very well understood, and methods of avoiding it are widely known (for example, use a 30-gauge needle in the lens and then aspirate the emulsified part of the cataract). Thus, in my cataract surgery population, I find that FLACS has no advantage over manual surgery in terms of efficacy and safety.
Of course, there are reimbursement factors to consider and I realize that, in the US, opting for FLACS will turn a cataract procedure into a refractive procedure and alter the billing pattern accordingly, which may be economically advantageous for the practice. Many countries outside the US, however, do not have such a system, and receive no income advantage from FLACS or even Zepto. In conclusion, at the risk of disappointing FLACS aficionados, I have to say that my experience of cataract surgery over 15 years is that FLACS is by no means definitively superior to manual techniques. Ethically, therefore – and to ensure the consistently good outcomes that are essential for a private practice to survive – I am unable to adopt FLACS as my routine method of cataract surgery at this point. I await further developments in femtosecond laser technology with interest!
- AJ Kanellopoulos et al., “Phacoemulsification and silicone foldable intraocular lens implantation in a patient with chronic sarcoid uveitis”, J Cataract Refract Surg, 21, 364 (1995). PMID: 8523273.
- AJ Kanellopoulos, EB Dreyer, “Postoperative infection following current cataract extraction surgery”, Int Ophthalmol Clin., 36, 97 (1996). PMID: 8989603.
- AJ Kanellopoulos et al., “Timolol gel versus acetazolamide in the prophylaxis of ocular hypertension after phacoemulsification”, J Cataract Refract Surg., 23, 1070 (1997). PMID: 9379379.
- AJ Kanellopoulos et al., “Dodick photolysis for cataract surgery: early experience with the Q-switched neodymium: YAG laser in 100 consecutive patients”, Ophthalmology, 106, 2197 (1999). PMID: 10571359.
- AJ Kanellopoulos, Photolysis Investigative Group, “Laser cataract surgery: A prospective clinical evaluation of 1000 consecutive laser cataract procedures using the Dodick photolysis Nd:YAG system”, Ophthalmology, 108, 649 (2001). PMID: 11297476.
- AJ Kanellopoulos, “All-laser bladeless cataract surgery, combining femtosecond and nanosecond lasers: a novel surgical technique”, Clin Ophthalmol, 1791 (2013). PMID: 24049439
- AJ Kanellopoulos, G Asimellis, “Corneal epithelial remodeling following cataract surgery: three-dimensional investigation with anterior-segment optical coherence tomography”, J Refract Surg, 30, 348 (2014). PMID: 24893360.
- AJ Kanellopoulos et al., “Digital pupillometry and centroid shift changes after cataract surgery”, J Cataract Refract Surg, 41, 408 (2015). PMID: 25661135.
- AJ Kanellopoulos, G Asimellis, “Clear-cornea cataract surgery: pupil size and shape changes, along with anterior chamber volume and depth changes. A Scheimpflug imaging study”, Clin Ophthalmol, 8, 2141 (2014). PMID: 25368512.
- AJ Kanellopoulos, G Asimellis, “Standard manual capsulorhexis / Ultrasound phacoemulsification compared to femtosecond laser-assisted capsulorhexis and lens fragmentation in clear cornea small incision cataract surgery”, Eye Vis (Lond), 3 (2016). PMID: 27478858.
- I Tanev et al., “Nanosecond laser-assisted cataract surgery: Endothelial cell study”, J Cataract Refract Surg, 42, 725 (2016). PMID: 27255249.
Director at the Laservision Eye Institute, Athens, and Clinical Professor in the Department of Ophthalmology at NYU School of Medicine, New York.