Building Castles for Kids
There’s no point in trying to make very young children accommodate the demands of standard visual field tests. Instead, let’s harness their natural inclinations through the power of video games
My interest in the problems posed by pediatric visual field assessment started many years ago, when I was a trainee in Manchester. I was helping in Cecilia Fenerty’s clinics; she had a specific interest in pediatric glaucoma, and it was clear that getting visual fields in these patients was almost prohibitively difficult. They had short attention spans, often poor concentration, and over all they just didn’t like doing the VF tests. One day after clinic, I came home from the clinic and found my nephew playing a computer game; I tried to engage with him, to converse, but he wouldn’t even look up from the screen! That’s when it struck me – if we could design a field test that worked like a computer game, we might finally be able to properly assess the visual function of very young patients.
That original concept stayed at the back of my mind for a while – but things came to a head a little later, when I was a fellow at Moorfields. I’d learnt to code much earlier, and I decided to develop a computer game that was actually a visual field test. I remember showing the prototype to Sir Peng Khaw – it was quite surreal watching the great man playing a child’s computer game that I’d designed – especially as he was very positive about it. So, with his encouragement, we proceeded to a feasibility study at Moorfields, which involved building a castle and testing the game with about 20 children. And that was the real breakthrough moment; we had parents in tears because they at last had some explanation for their child’s symptoms, some way of moving forward and learning to deal with the condition. At that point, I knew we had made something of potential real-world use.
Shortly afterwards, I moved back to Manchester, and began discussing the new test with Cecilia Fenerty, and two other specialists: David Henson, who has done a lot of work in visual fields, and Susmito Biswas, who is a pediatric ophthalmologist. It became clear that the new test needed to be more psychophysically robust – so that it could ensure that the targets were of the right size and in the right area; for example, the target size needed to be adapted for different subject ages. With the help of an NIHR grant, we set about addressing these issues; it took several years, and the very capable assistance of students and trainees, including Yanfang Wang, Marco Miranda and Zaria Ali. The whole study was coordinated by Sarah Robinson, despite her being very ill at the time. It took a great deal of work by many people over a long period – and, at the end of all that, it didn’t work!
Of course, we made some adjustments, but the test still didn’t perform as it should; ultimately, getting to where we wanted to be required a huge number of system iterations. People perhaps don’t realize how difficult it is to develop a computer game that is entertaining and engaging; games like Angry Birds look very simple, but there is a lot more behind them than you might think, especially with regard to the mechanics and psychology of the set-up. And we had the added complexity of not only making the game simple and engaging, but also making it function as a robust visual field test.

Figure 1. Caspar's Castle.
It’s just a game – or is it?
Tariq Aslam, David Henson and colleagues at the Manchester Royal Eye Hospital have developed a video game for children. A bit far removed from ophthalmology? No: “Caspar’s Castle” tests VF parameters in children for whom standard perimetry may be unsuitable. Their recent proof-of-principle study (1) demonstrates the feasibility of using the game in a clinical setting.
- Site: Pediatric Ophthalmology Outpatients Department, Manchester Royal Eye Hospital, UK.
- Subjects: 88 children (aged 4-12 years) with no eye pathology, and 21 children (aged 4-16 years) with ocular pathology (13 with congenital glaucoma, 7 with secondary glaucoma and 1 with neurological damage to a temporal lobe).
- Hardware: Thinkpad laptop (Lenovo, China); calibrated OLED display monitor (Sony PVM2541A, Sony Corporation, Japan) encased within a model castle with a viewing window. A button control on the laptop allows children to respond to central and peripheral targets of a game.
- Software: Video game in which children direct a character (“Prince Caspar”) to eliminate castle invaders; some invaders are presented to central vision, others to peripheral vision. Storyline, animation, graphics and music are all intended to appeal to children.
- Assessments: In healthy children, a single eye was assessed with Caspar’s Castle using peripheral stimuli of (a) normal intensity (45 children); or (b) reduced intensity (43 children). The intent was to mimic early /moderate glaucomatous visual defects, as per Brusini Glaucoma Staging System (2). In patients with eye pathology (21 children), Caspar’s Castle was compared with standard visual field assessment (also in a single eye) by means of a qualitative, empirical comparison by clinical pediatric glaucoma experts. In both cohorts, repeatability of the Caspar’s Castle system was assessed by performing two tests, 30 minutes apart.
- Results: VF tests in healthy children returned a value of 0.895 (95 percent CI, p<0.0001) for area under receiver-operator characteristic curve, with sensitivity of 81.4 and specificity of 88.89. Of the 21 children with eye defects, seven had also completed standard Humphrey’s field assessments: Caspar’s Castle test results correlated well with Humphrey test results in these children (all the pathologically abnormal Humphrey’s tests had corresponding visual field loss per Caspar’s Castle). Repeatability data were derived from all 106 children and indicated that Caspar’s Castle has a coefficient of repeatability of 6.9 (95 percent CI).
In conclusion, assessment of Caspar’s Castle in normal children shows that it has satisfactory repeatability and high diagnostic accuracy, even for early/moderate defects. The high level of specificity of Caspar’s Castle suggests that it is likely to be suitable for use as a screening test (because of its low frequency of false negatives). Furthermore, use of the test in children with real pathology indicates that it correlates well with the standard Humphrey’s test. With an average time of 6.5 minutes per test, Caspar’s Castle therefore may be a convenient and effective means of visual field assessment in young children.
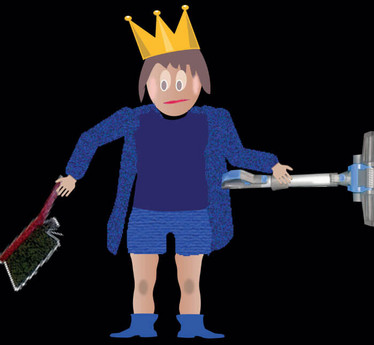
Figure 2. Prince Caspar.
With a lot of persistence, testing, me tweaking the game functionality and retesting, we eventually we ended up with the successful system we now have – Caspar’s Castle. In brief, the basis of the game is that a queen leaves her young son in charge of a castle; in her absence, the castle is invaded by little googly monsters, and it is the son’s job to get rid of these before the queen returns. The game has both a central component, to encourage good fixation, and a peripheral component to assess responses to non-central stimuli. It’s not just theoretical – we have now demonstrated the game’s diagnostic validity as a visual field-testing system in a study involving over 100 children (see It’s just a game – or is it?). Furthermore, we’ve been able to get good readings from children as young as four, and from other children with learning difficulties. That’s the power of a well-designed game – it’s so intuitive, it just draws the children in. And the really nice thing is that it’s a visual field test that the kids – both boys and girls – actually enjoy doing!
Fresh fields, pastures new
It has been quite a long and involved journey – six or seven years of development – but we got there in the end. And we don’t want this to be the end of it; there’s no point in developing a system like this and then leaving it on the shelf. We want it to be out in the real world, getting used in clinics and making a difference to patients. For that to happen, we need partners with complementary expertise, particularly manufacturers of visual field tests that use an LCD or OLED screen; all we’d need to do is provide them with the Caspar’s Castle software, and their systems would be suitable for pediatric VF testing. There are still some regulatory hurdles to jump through, like CE marking, but again, this is where the right partner could help. We’d be really interested in hearing from new contacts – if there are any companies out there with computer screen-based visual field tests, the University of Manchester Intellectual Property Department wants to talk to you!
Special Cases: SVOP Overview from The Ophthalmologist editor
CNS tumors are the most common cancers of childhood, and a significant percentage of these impinge on the visual pathway. But how can we objectively assess visual field defects in young children who may neither recognize their own visual field defect nor be mature enough – or well enough – to correctly perform standard tests? Robert Minns’ answer to this problem was to develop saccadic vector optokinetic perimetry (SVOP). This system exploits eye-tracking technology to automatically recognize when a child detects the visual field stimulus – a cartoon character – and therefore may be less susceptible to errors arising from either examiner or subject. The main features of SVOP are as follows:
- Hardware: PC, patient display (Dell 2005FPW 20” liquid crystal display), eye tracker (Tobii Technology: X50 or IS-1)
- Pre-SVOP calibration of patient gaze: (i) measure eye characteristics while patient follows moving visual stimulus (cartoon character); (ii) use measurements in context of mathematical model of eye to calculate gaze position
- Apply multi-fixation target strategy and eye-tracking technology to monitor eye movements and fixations in response to visual field stimuli:
- Fixation targets of 1.5-degree angular diameter
- Real-time tracking allows system to remove fixation target and introduce VF stimulus as soon as target is fixated by child
- VF stimuli of size Goldmann III, duration 200 ms; stimulus luminance 137 cd/m2; background luminance 10 cd/m2
- Software algorithm analyses direction and amplitude of saccades over the 1 second window following stimulus presentation
- VF stimuli that are undetected in two separate tests, according to saccade analysis, are recorded as ‘unseen’.
- System continuously monitors the child’s head position and adjusts according to movements, so as to present stimuli at defined visual field locations (i.e., no requirement for chin-rest)
- Responses to visual field stimuli are automatically recorded – no need for child to understand the test, push a button or otherwise react.
In theory, this new system does not require the child to remain still, maintain fixation on a single target, or consciously report a visual field stimulus. But does it work in the real world? Initial results are encouraging: SVOP has been shown to be comparable with Humphrey standard automated perimetry in adults (3, 4), and now Minns and colleagues report promising results from a comparison of SVOP with other methods in a series of children with brain tumors (5). In brief:
- Patients recruited at Royal Hospital for Sick Children in Edinburgh, from April 2008-August 2013
- 16 patients (mean age 7.2 y, range 2.9 - 15 y, seven male, nine female); of which 12 patients (75 percent) successfully performed SVOP testing
- SVOP results were compared with a consensus view of the likely visual field patterns (as determined by an expert panel on the basis of clinical findings, neuroimaging and, where possible, other forms of visual field assessment):
- SVOP sensitivity – 100 percent
- SVOP specificity – 50 percent (80 percent positive predictive value and 100 percent negative predictive value)
- SVOP visual field plots agreed with expected visual fields
- 6 patients were tested with both Goldmann perimetry and SVOP: these all showed similar visual fields
- Conclusion: SVOP is a highly sensitive test that can characterize the central 30 degrees of visual field in greater detail than other techniques applicable to young children with brain tumors.
The ability of SVOP to accurately characterize the nature and extent of visual field defects in very young children – including those with brain tumors – sets it apart from standard perimetry and many existing alternatives. Future work in this area may include testing SVOP repeatability and reliability in the long-term follow-up of a cohort of children to assess its ability to monitor disease progression and treatment response.
- TM Aslam et al., “Diagnostic performance and repeatability of a novel game-based visual field test for children”, Invest Ophthalmol Vis Sci, 59, 1532-1537 (2018). PMID: 29625475.
- P Brusini and S Filacorda, “Enhanced glaucoma staging system (GSS 2) for classifying functional damage in glaucoma”, J Glaucoma, 15, 40-46 (2006). PMID: 16378017.
- IC Murray et al., “Feasibility, accuracy and repeatability of suprathreshold saccadic vector optokinetic perimetry”, Transl Vision Sci Technol, 5, 15 (2016). PMID: 27617181.
- AD McTrusty et al., “Comparison of threshold saccadic vector optokinetic perimetry (SVOP) and standard automated perimetry (SAP) in glaucoma. Part II: Patterns of visual field loss and acceptability”, Transl Vis Sci Technol, 6, 4 doi: 10.1167/tvst.6.5.4 (2017). PMID: 28900577.
- IC Murray et al., “Detection and characterisation of visual field defects using Saccadic Vector Optokinetic Perimetry in children with brain tumours”, Eye, 32, 1563 (2018). PMID: 29880917.
- IC Murray et al., “Saccadic vector optokinetic perimetry (SVOP): novel technique for automated static perimetry in children using eye tracking”, Conf Proc IEEE Eng Med Biol Soc (EMBC), 2013, 3186 (2013). PMID: 24110405.
Tariq Aslam is a Reader at the University of Manchester and a consultant ophthalmologist at Manchester Royal Eye Hospital. He is the Director of the Manchester Investigative Ophthalmology and Vision Science MSc course, Director of the Manchester undergraduate Ocular Disease course, Editor of Eye News and Ophthalmology and Therapy and Associate Editor of Acta Ophthalmologica.