The Economics of Gene Therapy
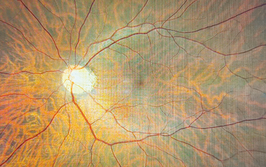
Gene and stem cell therapies hold the promise of restoring vision in patients with retinal diseases – but who should be paying for these treatments, and how?
At a Glance
- As they advance through clinical trials, gene therapies are coming closer and closer to reality for patients with retinal diseases
- But with approaching treatments come approaching costs, and gene therapies can cost as much as US$1 million for a single treatment
- Especially in disorders with small patient populations, like many ocular diseases, the price per dose of a new therapy must be high – which can prevent patients from accessing it
- I propose a model of annuity payments for gene and stem cell therapies that would charge based on both the duration of treatment and the degree of efficacy

Gene therapy looks like it will transform the treatment of a number of ophthalmic diseases in the near future. Clinical trials in a number of retinal diseases, including Leber congenital amaurosis (LCA), the wet form of AMD, Stargardt disease/ Stargardt’s macular dystrophy (SMD), and Usher Syndrome 1b have shown promising results, with gene therapy providing some vision improvement for most who received it, without causing significant safety concerns. Of course, some questions about gene therapy still remain – will it deliver Ricki Lewis’ holy grail of “the forever fix” (1), or something less? And, with the first Western world approval of a gene therapy treatment – Glybera (alipogene tiparvovec) for lipoprotein lipase deficiency (LPLD) – having been gained, will ophthalmic therapies be next?
But these aren’t the only questions being asked. As ophthalmic gene therapy approaches marketing approval, likely within the next 2–3 years, one of the most significant concerns is cost. Glybera treatment may cost as much as $1.6 million per patient (2) but the extent of its worldwide market numbers in the hundreds – this is whole orders of magnitude smaller than the potential market size of the ophthalmic diseases currently under investigation. Nobody expects any of the proposed ophthalmic treatments to cost that much, as most of the disorders to be treated have much larger patient populations, but that unanswered question remains. What will ocular gene therapy (and, perhaps, stem cell treatment) cost? And how will patients and the medical community pay for it?
A pricing proposal
As a former consultant to the ophthalmic industry, I frequently put together models predicting where an ophthalmic technology might go – for instance, models for how laser refractive surgery (which I did four years before marketing approval), or intraocular lenses (in a private company’s worldwide report on the use of this technology) might penetrate the market. So preparing a pricing model for a new technology is familiar ground for me. To create this one, I made several assumptions (see Box 1), along with proposing a pricing model based on the likely population of eyes to be treated. I started with a reasonable pricing model for Glybera, based on the reported price per treatment and the estimated population to be treated (3). Next, I estimated the populations of people likely to need treatment for a variety of retinal disorders, including for LCA, SMD, retinitis pigmentosa (RP), wet AMD, and also dry AMD. These estimates and proposed pricings for potential stem cell or gene therapy treatments are shown in Table 1.
| Estimated Population to be Treated | Proposed Price Per Dose | Yield | Examples |
| Several hundred (100 - 300) | $1M | $100M - $300M | Glybera for LPLD, Specific genes for Leber Congenital Amaurosis |
| Several thousand (1,000 - 3,000) | $500,000 | $500M - $1.5B | Stargardt Disease |
| Several tens of thousand (30,000 - 50,000) | $100,000 | $3B - $5B | Retinitis Pigmentosa |
| Several million (1M - 3M) | $50,000 | $50B - $150B | Wet AMD |
| Multiple million (8M - 9M) | $35,000 | $290B - $320B | Dry AMD |
Box 1. Model assumptions.
- Gene Therapy is to be a one dose treatment (“The Forever Fix”) to fix/correct the gene deficiency/defect causing the disease state.
- The case for using stem cell therapy for dry AMD (and SMD), is based on Ocata data to date; one treatment has maintained increased vision for more than 2 years in their clinical trials.
- The above pricing is for a “for profit” business entity, seeking to reclaim its research and clinical trial expenses, and to make a profit for shareholders. It would be expected that a non-profit or humanitarian entity would charge, perhaps, 1/10 to 1/3 of the prices noted.
Estimates of populations to be treated: LCA – incidence of 1 in 80,000, or a U.S. population of about 3 million, but only 300–500 per specific gene. Stargardt – incidence of about 1 in 15,000, or a U.S. population of 15 to 20 million, but only about 35,000 – 40,000 are expected to be treated. Both stem cell and gene therapy treatments are in clinical trials. Retinitis Pigmentosa – incidence of about 1 in 3000 – 5000, or a U.S. population of about 62,500, of which perhaps half might be treated. Wet AMD – about 1.6 million to 1.8 million in the U.S. All might be treatable if gene therapy works. Dry AMD – about 8 million to 9 million estimated in the U.S. with intermediate to advanced stages, most of whom could be treatable, if it would preclude progression of vision loss and advancement to the wet form. Stem cell therapy treatments are in clinical trials. Data source – Market Scope estimates based on data from NIH and NIE. (Link: top.txp.to/0515/AMDcauses)
Planning for payment
Luckily, when coming up with a proposed method for paying for these high-priced treatment modalities, I didn’t have to reinvent the wheel. That hard work has been done by others before me. The discussion started last year with an Xconomy article by Luke Timmerman (4). He noted, “As a follower of gene therapy for the past dozen years, it’s fascinating to me that the conversation is moving in this direction. Scientists have been telling us about gene therapy and the yellow brick road to cures for more than 20 years, but none have yet made it all the way to FDA approval […] For years, the savviest executives and investors inside biotech wondered: Is gene therapy safe enough? Will it ever work? Even if it works, will the FDA ever stick its neck out and approve one?”
Timmerman went on to say, “There is, of course, a neverending debate about the ethics of drug pricing. When a cancer drug extends life for a few months, works for a fraction of patients, and a company still charges US$100,000, it’s understandably controversial. When a new drug comes along that’s life-altering, especially for young people, that’s a whole different story. If, for example, UniQure – the supplier of Glybera, opts for a long-term payment installment plan, you can imagine some complex questions.” These questions span a wide range of concerns – how to measure the effectiveness of the drugs, what tests (especially invasive procedures) to order and how often, who was responsible for payment, what happened if patients switched insurance providers, and what to do if a particular treatment was unusually successful or, conversely, failed before being paid for in full. Clearly, long-term payment plans, despite their potential benefits, were not the answer.
Then, later that year, Troyen Brennan and James Wilson provided a potential answer – an annuity payment plan (5). They wrote in Nature Biotechnology, “We suggest an alternative approach to a high, single payment, whereby value is captured through annuity payments received over a specified period based on evidence that the treatment continues to be effective.” In their opinion, a one-time payment may be simple in terms of administration, but complex in terms of the practical and policy risks involved. For instance, they suggest that – as gene therapy products will be approved based on short-term trial data – patients and insurers might be reluctant to make a lump sum payment based on the projected duration of their treatment’s efficacy. They also point out that, given the current trend toward reducing healthcare costs, novel treatments with price tags in excess of US$1 million might face strong criticism. Although the authors do state that “truly effective gene therapy treatments may reduce the overall financial burden to the healthcare system,” they warn that gene therapy breakthroughs may face substantial obstacles if reimbursement is not thoughtfully structured in advance of their emergence.
The authors also point out that, at least in the United States, the context for what is essentially a “pay-as-you-go model” may already exist. “If gene therapy is the standard of care,” they write, “then qualified plans may be required to offer it as part of the minimum essential benefits package.” And ever since the Patient Protection and Affordable Care Act – “ObamaCare” – was passed, health insurance plans in the US can no longer either limit lifetime benefits or discriminate based on disease. This means that, in theory, a patient could continue gene therapy – with an annual fee paid by the insurance provider – for as long as the treatment was effective (or up to a predetermined amount equivalent to a discount on an existing therapy). Patients who changed insurers, or whose providers ceased to offer the appropriate policies, would be able to switch to other qualified plans that would accept both the patient and the gene therapy annuity fee.
“In some ways,” Brennan and Wilson conclude, “the critical issue will be the calculation of the original price, one that other successor insurers would presumably have to honor. This might be solved by the government, which, because many of the patients with rare diseases are disabled and thus qualify for Medicare, would have to set a Medicare price. The Medicare precedent could set a reference price for the commercial market, and very small revisions to federal law could guarantee that successor insurers would honor the Medicare pricing set by an original insurer.” So it appears that we might indeed have a payment model for high-cost gene therapy (and stem cell) treatment of ocular diseases.
Paying for performance
In conversation with those involved in the biotechnology industry, I’ve heard the suggestion that gene and stem cell therapy should be priced not only on the basis of patient population, but also according to performance. “As with any other drug or treatment,” one expert said, “one particular gene therapy won’t necessarily work for everyone with a certain disease, and it doesn’t make sense to pay US$500,000–1 million only to find out that the treatment actually doesn’t work for you.” The price, this expert said, should depend on both the degree and the duration of efficacy – not all gene therapies are equal; some are true one-shot cures, while others provide benefits like stopping progression of the disease for a variable length of time. For example, Avalanche Biotechnologies’ (Menlo Park, CA, USA) gene therapy-based wet AMD drug won’t cure the disease, but it will help to substantially reduce the number of anti-VEGF injections needed by a patient. “In general,” he said, “I really like the annuity model, which seems to address the pay-for-performance and duration of efficacy issues.”
A system of annuity payments would pose fewer implementation problems in regions with single-payer systems like those found in Europe. In areas with multiple healthcare providers, like the United States, implementing such a system could be more challenging – but, ultimately, offer the reward of giving patients access to ophthalmic disease therapies that could make a real and ongoing difference to their vision.
Irv Arons reports on new drugs and devices for the treatment of retinal diseases. A former consultant to the ophthalmic and medical laser industries with management consultants Arthur D. Little for 25 years, Irv ran his own company, Spectrum Consulting, for 11 years before his retirement.
- R Lewis, “The Forever Fix: Gene Therapy and the Boy Who Saved it”, St. Martin’s Press (New York) (2012).
- J Whalen, “Gene-Therapy Approval Marks Major Milestone”, The wall street journal (2012). Available at: on.wsj.com/1Oftq95. Accessed April 22, 2015.
- C Morrison, “$1-million price tag set for Glybera gene therapy”, Trade Secrets Blog, Nature, March 3, 2015. Available at: bit.ly/glybera1milliony. Accessed April 27, 2015.
- L Timmerman, “Gene therapy lurches ahead, sees thorny future questions on price”, Xconomy(2014). Available at: bit.ly/1iD2MGy. Accessed April 22, 2015.
- TA Brennan, JM Wilson, “The special case of gene therapy pricing”, Nat Biotechnol, 32, 874–876 (2014). PMID: 25203033
Irv Arons’ Journal is a well-read blog that reports on new drugs and devices for the treatment of retinal diseases, including age-related macular degeneration (AMD). Until his retirement, Irv was a consultant to the ophthalmic and medical laser industries, working for management consultants Arthur D. Little for 25 years and running his own company, Spectrum Consulting, for 11 years.